
Covid-19 updated 1/6/2023
The webpage is divided into 10 parts:
Part 0a) Recently updated information: Including Delta & Omicron variant and ramifications
Information below
Denmark vs USA policy on covid
13 Things To Know About Paxlovid, the Latest COVID-19 Pill
Ivermectin
Myocarditis (the vaccine and covid)
Immune-mediated hepatitis (vaccine and covid)
COVID-19 as a primarily vascular disease
hospitalized COVID-19 patients
ACS Risk Biomarkers Significantly Increase After mRNA COVID-19 Vaccine
Comparing SARS-CoV-2 natural immunity to vaccine-induced immunity
Recent research (below) reveals that one single dose of the m-RNA vaccines appears to be very effective at preventing the severe form of covid-19 and that if you had covid-19 that the vaccine does not necessarily benefit from vaccination
PCR testing update
There is a lot of science-based information on how viruses, like covid-19, mutate to variants that are more infectious but not necessarily more deadly to raise the probability of their continued existence in a given target host like humans.
Part 1) Introduction plus:
a)Typical covid-19 progression for people, who exhibit symptoms
b) Normal Chest X-ray Doesn't Rule Out COVID-19
c)What happens in the ER and ICU and how that may need to change for a better patient outcome.
d) ICU change of protocol to less harmful methods
e) A brief summary of three different theories of how covid-19 affects the body in severe cases and how this affects the ICU (Intensive Care Unit) treatment of patients.
f)Six months plus, of coronavirus: the mysteries scientists are still racing to solve
Part 2)
Relevant statistics to Covid-19 and the ICU.
Details of tests to detect covid-19 and tests to detect antibodies to covid-19
Blood chemistry test results for covid-19 patients
The question: When will it be over? is answered by scientists, including the methods of prediction.
The Risks - Know Them - Avoid Them
The science of airborne spread of covid
Part 3) A detailed look at current ICU treatment, to a degree based on the assumption the virus directly adversely affecting the lungs, which causes a cytokine storm causing the destruction of the lungs and then resulting hypoxia.
Part 4)
A)
A somewhat detailed look at how the virus might be causing extreme hypoxia (lack of oxygen) and death, if viral proteins are interfering with hemoglobin's role in oxygen transport, and if this occurs before the cytokine storm and the destruction of the lungs and other organs.
B) An altered less invasive ICU protocol, from standard ICU treatment, if this is the case.
C) A newer theory, also related to the virus and blood, is that the covid-19 is invading endothelial cells and causing numerous blood clots, including, in some cases, large clots in the brain.
Part 5)
Day by Day narration of a previously healthy 40 year old women, who was covid-19 positive. This person had many somewhat typical symptoms of phase one then her body advanced to some severe ones experienced in phase 2 of the infection.
Part 6)
If you have survived being infected by covid-19, are you now immune to being reinfected? Not necessarily.
Recent research on covid-19 immunity, plus a new stain of covid-19 confounds the problem.
Plus do your genes make a difference in susceptibility and/or severity of the disease?
Part 7)
Drugs currently undergoing clinical trials for treating covid-19
Plus, Related to Covid-19 Vaccine Development
Part 8)
a)5 ways coronavirus could help humanity survive the ecological crisis
b)The covid-19 virus is attempting to teach us a lesson, about how we live.
c)CORONAVIRUS - The Uncomfortable Truth -- 8 minute video
d)Zach Bush MD a video interview worth viewing, somewhat different than the traditional view and more holistic in approach.
e)Biological weapons virus gain of function (GOF) research
f) Profile of a killer: the complex biology powering the coronavirus pandemic
g) Chief Science Officer for Pfizer Says "Second Wave" Faked on False-Positive COVID Tests
Part 9)
Some lesser known details about Hand Washing. Mask wearing (positive and negative details), Face Shields, due to covid-19.
VigiBase is the unique WHO global database of reported potential side effects of medicinal products. It is the largest database of its kind in the world, with over 28 million reports of suspected adverse effects of medicines, submitted, since 1968, by member countries of the WHO PIDM. It is continuously updated with incoming reports.
https://who-umc.org/vigibase/
access to database: http://vigiaccess.org
Part 0a) Recently updated information
If one wades through all the recent information on this site, related to covid and the vaccines: A reasonable conclusion might be that covid-19 is a serious decease and the USA vaccines for people over 50 years of age, almost unambiguously lower your chance of dying from covid, and if you are 18 and under, the vaccines increase your chance of dying from the vaccine more than a covid infection.
This is part of the reason that Denmark, with generally better health care statistics than the USA has recently changed their policy on covid vaccines in the following way:
October 2022
The Danish Health Authority is offering COVID-19 booster shots to people at a higher risk of severe illness: people 50 and older; vulnerable people younger than 50; relatives of vulnerable people; and anyone who works in health care and elderly care.
The COVID-19 primary vaccine series is generally still available to people younger than 50, though vaccinations have been limited among children. Starting in July, it was no longer possible for children younger than age 18 to get a first COVID-19 shot and after August, it was no longer possible for them to get a second injection. Children at high risk of becoming severely ill can still get a vaccine at their doctor’s recommendation, according to the health authority.
https://www.politifact.com/
https://www.mylifeelsewhere.com/compare/united-states/denmark
13 Things To Know About Paxlovid, the Latest COVID-19 Pill
BY KATHY KATELLA November 29, 2022
https://www.yalemedicine.org/news/13-things-to-know-paxlovid-covid-19
Administration approved Pfizer’s Paxlovid, a protease inhibitor ,which means it blocks an enzyme needed for viral replication. The drug showed an impressive 88 percent efficacy in preventing hospitalization among unvaccinated patients —
The FDA has approved monoclonal antibodies as a treatment for Covid-19 patients at risk of progressing to severe disease. It recently expanded this approval to include monoclonal antibodies for children as well. The catch is this treatment has to be administered in a clinic or hospital, as an IV infusion or as four shots — but against past waves of Covid it has been highly effective, with one high-quality study finding an 85 percent reduction in the risk of hospitalization or death.
Research currently published only in preprints suggests that, based on lab studies of antibody neutralization, 18 of the 19 different specific antibody formulations examined are less effective in fighting off omicron. There’s one notable exception: Sotrovimab, a monoclonal antibody from GlaxoSmithKline and Vir Biotechnology, seems to hold up well against omicron.
Ivermectin, touted as a miracle cure, has shown mostly small effects in trials
https://www.vox.com/future-perfect/22841852/covid-drugs-antibodies-fluvoxamine-molnupiravir-paxlovid
Ivermectin for COVID-19: real-time meta analysis of 73 studies
https://ivmmeta.com/
‘Science is flawed’: COVID-19, ivermectin, and beyond
....A meta-analysis of ivermectin, which is usually considered the gold standard of research practices, found a huge benefit for the drug. However, the paper has not been corrected, even though the studies underlying its results were found to be likely fraudulent. ....
https://www.medicalnewstoday.com/articles/science-is-flawed-covid-19-ivermectin-and-beyond
Ivermectin and Molnupiravir: How does the widely used drug compare to the new drug in treating Covid-19?
https://www.todayville.com/ivermectin-and-molnupiravir-how-does-the-widely-used-drug-compare-to-the-new-drug-in-treating-covid-19/
January 25, 2022 from the Journal of the American Medical Association
Myocarditis Cases Reported After mRNA-Based COVID-19 Vaccination in the US From December 2020 to August 2021
Matthew E. Oster, MD, MPH1,2,3; David K. Shay, MD, MPH1; John R. Su, MD, PhD, MPH1; et al
What is the risk of myocarditis after mRNA-based COVID-19 vaccination in the US?
In Summary:
Findings In this descriptive study of 1626 cases of myocarditis in a national passive reporting system, the crude reporting rates within 7 days after vaccination exceeded the expected rates across multiple age and sex strata. The rates of myocarditis cases were highest after the second vaccination dose in adolescent males aged 12 to 15 years (70.7 per million doses of the BNT162b2 vaccine), in adolescent males aged 16 to 17 years (105.9 per million doses of the BNT162b2 vaccine), and in young men aged 18 to 24 years (52.4 and 56.3 per million doses of the BNT162b2 vaccine and the mRNA-1273 vaccine, respectively).
....
Meaning Based on passive surveillance reporting in the US, the risk of myocarditis after receiving mRNA-based COVID-19 vaccines was increased across multiple age and sex strata and was highest after the second vaccination dose in adolescent males and young men.
....
The primary outcome was the occurrence of myocarditis and the secondary outcome was pericarditis.
https://jamanetwork.com/journals/jama/fullarticle/2788346
Published: September 6, 2022
Myocarditis from COVID-19 booster rare, but risk highest among teen boys, young men
By American Heart Association News
...
"It is important to understand the connections between this rare heart condition and COVID-19 vaccines so we can monitor the prevalence of myocarditis and pay extra attention to those who are most at risk," lead study author Dr. Dror Mevorach said in a news release. He is a professor of medicine and head of the Immunology-Rheumatology Institution at Hadassah Ein Karem Medical Center in Jerusalem and chairman of the Israeli Ministry of Health Committee for Identifying Myocarditis as an Adverse Effect of mRNA Vaccines.
Myocarditis is an inflammation of the middle layer of the wall of the heart muscle, called the myocardium. It can be triggered by a viral infection and can weaken the heart muscle and the heart's electrical system, which makes it harder for the heart to beat normally. The condition can resolve on its own or with treatment, but also can cause lasting damage to the heart.
Previous research from public health agencies around the world, including the U.S. Centers for Disease Control and Prevention, has shown a potential increased risk of myocarditis following an mRNA COVID-19 vaccine. A recent study published by the Ministry of Health in Israel found a low incidence of myocarditis after a first and second dose of Pfizer's vaccine. But because risk was highest among young men and teen boys who had a second dose of the vaccine, researchers were concerned about the potential effect a third dose, the booster dose.
....
https://www.heart.org/en/news/2022/09/06/myocarditis-from-covid-19-booster-rare-but-risk-highest-among-teen-boys-young-men
Published: August 22, 2022
COVID-19 infection poses higher risk for myocarditis than vaccines
By American Heart Association News
...
The analysis showed people infected with COVID-19 before receiving a vaccine were 11 times more at risk for developing myocarditis within 28 days of testing positive for the virus. But that risk was cut in half if a person was infected after receiving at least one dose of a COVID-19 vaccine.
The risk for myocarditis increased after receiving the first dose of the AstraZeneca vaccine, and after a first, second and booster dose of the Pfizer or Moderna vaccine. But the risk of myocarditis associated with the vaccine was lower than the risk associated with COVID-19 infection before or after vaccination – with one exception. Men under 40 who received a second dose of the Moderna vaccine had a higher risk of myocarditis following vaccination. The Pfizer and Moderna mRNA vaccines are available in the U.S.
...
J Hepatol. 2021 Oct 5
doi: 10.1016/j.jhep.2021.09.031
PMCID: PMC8491984 PMID: 34619252
Immune-mediated hepatitis with the Moderna vaccine, no longer a coincidence but confirmed
Gloria Shwe Zin Tun,∗ Dermot Gleeson, Amer Al-Joudeh, and Asha Dube
"We have read with interest the recent cases suggesting the possibility of vaccine-induced immune-mediated hepatitis with Pfizer-BioNTech and Moderna mRNA-1273 vaccines for the SARS-CoV-2 virus.[1], [2], [3], [4], [5], [6], [7] However, as the cohort of vaccinated individuals against COVID-19 increases, the previously reported cases could not exclude a coincidental development of autoimmune hepatitis, which has an incidence of 3/100,000 population per year.8 Our case demonstrates conclusive evidence of vaccine-induced immune-mediated hepatitis with a rapid onset of liver injury after the first Moderna dose, which on re-exposure led to acute severe autoimmune hepatitis."
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8491984/
The novel coronavirus’ spike protein plays additional key role in illness
Salk researchers and collaborators show how the protein damages cells, confirming COVID-19 as a primarily vascular disease
https://www.salk.edu/news-release/the-novel-coronavirus-spike-protein-plays-additional-key-role-in-illness/
Nearly 60% of hospitalized COVID-19 patients in Israel fully vaccinated, data shows
https://www.beckershospitalreview.com/public-health/nearly-60-of-hospitalized-covid-19-patients-in-israel-fully-vaccinated-study-finds.html
Coronavirus vaccines work. But this statistical illusion makes people think they don’t.
In Israel for a time, more vaccinated people were hospitalized for covid-19 than unvaccinated people. There’s no reason to worry.
https://www.washingtonpost.com/outlook/2021/08/31/covid-israel-hospitalization-rates-simpsons-paradox/
ACS Risk Biomarkers Significantly Increase After mRNA COVID-19 Vaccine
https://www.thecardiologyadvisor.com/home/topics/acs/acute-coronary-syndrome-acs-biomarkers-mrna-covid19-vaccine/
The risk of developing acute coronary syndrome (ACS) significantly increased in patients after receiving mRNA COVID-19 vaccines, according to a report presented at the American Heart Association (AHA) Scientific Sessions 2021, held from November 13 to 15, 2021.
The study included 566 men and women (1:1) aged 28-97 years, who were patients in a preventive cardiology practice. All patients received a new PULS Cardiac Test 2-10 weeks after their second COVID-19 vaccine. This test result was compared with a PULS score from 3-5 months prevaccination. The PULS Cardiac Test measures multiple protein biomarkers, including hepatocyte growth factor [HGF], soluble Fas, and IL-16, and uses the results to calculate a 5-year risk score for new ACS. The PULS score increases with above-normal elevation. All participants received this test every 3-6 months for 8 years.
From prevaccination to postvaccination, the levels of IL-16 increased from 35=/-20 to 82=/-75 above the norm. Soluble Fas showed an increase from 22±15 to 46=/-24 above the norm. HGF rose from 42±12 to 86±31 above the norm. As a result, the 5-year ACS PULS risk score increased from 11% to 25%. By the time the report was published, changes had persisted for 2.5 months or more after the second vaccine dose.
The study author concluded that “mRNA [vaccines] dramatically increase inflammation on the endothelium and T cell infiltration of cardiac muscle and may account for the observations of increased thrombosis, cardiomyopathy, and other vascular events following vaccination.”
Above primary source:
Abstract 10712: Mrna COVID Vaccines Dramatically Increase Endothelial Inflammatory Markers and ACS Risk as Measured by the PULS Cardiac Test: a Warning
Steven R Gundry MD
Originally published8 Nov 2021Circulation. 2021;144:A10712
https://www.ahajournals.org/doi/10.1161/circ.144.suppl_1.10712
https://www.coronavirustoday.com/2021/11/22/mrna-covid-19-vaccination-increases-endothelial-inflammatory-markers-and-acs-risk
Critiques and more detailed studies related to the above study
https://www.tctmd.com/news/questions-raised-about-study-linking-mrna-vaccines-increased-acs-risk
Do mRNA COVID-19 Vaccines Increase Heart Disease Risk?
https://www.techarp.com/science/mrna-vaccines-heart-disease-risk/
Myocarditis after Covid-19 Vaccination in a Large Health Care Organization
https://www.nejm.org/doi/full/10.1056/NEJMoa2110737
August 4, 2021
Myocarditis and Pericarditis After Vaccination for COVID-19
George A. Diaz, MD1; Guilford T. Parsons, MD, MS2; Sara K. Gering, BS, BSN3; et al
https://jamanetwork.com/journals/jama/fullarticle/2782900
Dr. Robert Malone (co-inventor of mrna vaccines) speaks out about scientific censorship related covid-19 link
The Delta Variant of covid-19 virus appears to be approximately 80% of the covid cases in America as of early August 2021.
https://health.ucdavis.edu/coronavirus/covid-19-information/delta-variant.html
The current covid vaccines used in the USA still appear about 90% effective in preventing the severe form of covid-19, which can lend to intensive hospitalization. It appears that the vaccines effectiveness starts waning significantly by 7 months. These same vaccines increasingly appear to be less effective in preventing non-severe delta covid-19 infections in already vaccinated people (Breakthrough infections).
Comparing SARS-CoV-2 natural immunity to vaccine-induced immunity: reinfections versus breakthrough infections
Sivan Gazit, Roei Shlezinger, Galit Perez, Roni Lotan, Asaf Peretz, Amir Ben-Tov, Dani Cohen, Khitam Muhsen, Gabriel Chodick, Tal Patalon
doi: https://doi.org/10.1101/2021.08.24.21262415
https://www.medrxiv.org/content/10.1101/2021.08.24.21262415v1
Conclusions This study demonstrated that natural immunity confers longer lasting and stronger protection against infection, symptomatic disease and hospitalization caused by the Delta variant of SARS-CoV-2, compared to the BNT162b2 two-dose vaccine-induced immunity. Individuals who were both previously infected with SARS-CoV-2 and given a single dose of the vaccine gained additional protection against the Delta variant.
A recent example of breakthrough infections is what occurred in Provincetown, Mass. where:
“According to the report, of the 469 people included in the study who were in the area between July 3 and July 17 and tested positive for the coronavirus, 74% were fully vaccinated. A total of five people were hospitalized, four of them vaccinated, and there were no deaths. 90% of the subset of people who had sequencing performed on their samples were infected with the delta variant.”
https://www.factcheck.org/2021/08/scicheck-posts-misinterpret-cdcs-provincetown-covid-19-outbreak-report/
This trend of breakthrough infections of the already vaccinated, or people have already had covid-19 appears to be similar, in both cases the symptoms usually are mild or asymptomatic and in both cases the individuals can spread covid-19.
The above does not portend well for achieving herd immunity, where covid-19 dies out due to lack of people who can carry the infection.
The delta variant of the coronavirus appears to cause more severe illness than earlier variants and spreads as easily as chickenpox, according to an internal federal health document that argues officials must “acknowledge the war has changed.” ... from internal CDC document
...
It cites a combination of recently obtained, still-unpublished data from outbreak investigations and outside studies showing that vaccinated individuals infected with delta may be able to transmit the virus as easily as those who are unvaccinated. Vaccinated people infected with delta have measurable viral loads similar to those who are unvaccinated and infected with the variant.
https://www.washingtonpost.com/health/2021/07/29/cdc-mask-guidance/
1) CDC data shows the vaccines have low efficacy against transmission of Delta, a variant that the vaccines were not designed for.
At the end of July 2021, the CDC decided that everyone indoors should wear masks again https://www.cnn.com/2021/07/30/health/breakthrough-infection-masks-cdc-provincetown-study/index.html , based on a study of Barnstable county in Massachusetts which found that 74% of COVID cases occurred in those who were vaccinated, even though 69% of eligible people in the county had the shots. 89% of the cases were Delta and the vaccinated people were spreading the delta variant as much as the unvaccinated. If this study has this much significance, then other data from this study should be considered significant also. This is the study Outbreak of SARS-CoV-2 Infections, Including COVID-19 Vaccine Breakthrough Infections, Associated with Large Public Gatherings — Barnstable County, Massachusetts, July 2021 | MMWR (cdc.gov) , and below are the other findings which have not been publicized in the media.
Data from the study:
People Cases Cases/People Hospitalizations % of total Hosp. Deaths % of Cases Hosp.
Unvac. 66,030 (31%) 123 (26%) 123/66,030 = 0.186% 1 (age 50-59, 1 pre-exist. condition) 1/5 = 20% 0 1/123 = 0.8%
Vac. 146,970 (69%) 346 (74%) 346/146,970 = 0.235% 4 (age 20-70, 2 pre-exist. condition) 4/5 = 80% 0 4/346 = 1.2%
================================================================================================================
Total 213,000 469 (100%) 469/213,000 = 0.220% 5 0 5/469 = 1.06%
================================================================================================================
Total 213,000 469 (100%) 469/213,000 = 0.220% 5 0 5/469 = 1.06%
a) The number of Delta cases among the vaccinated are 26% higher than the unvaccinated.
The population of Barnstable county is 213,000, and the study reports that 69% of its population is vaccinated, = 146,970 people; 31% is unvaccinated, = 66,030 people
Unvac cases/person = 123/66,030 = 0.186%
Vaccinated cases/person = 346/146,970 = 0.235%, which is 26% higher than 0.186%
So the Delta case rates in the vaccinated are not better than the unvaccinated, and the shots may be increasing the Delta case rate.
This contradicts CDC statements that breakthrough cases are rare, and that vaccination reduces the spread.
Clearly the vaccinations are not reducing breakthrough Delta cases or Delta spread.
b) 80% of the total hospitalized for COVID were vaccinated, while 20% were not vaccinated.
This also contradicts recent CDC and Fauci reports that 95% of hospitalized COVID cases are in the unvaccinated.
c) The hospitalization rates for vaccinated (1.2%) and unvaccinated (0.8%) cases are about the same, maybe higher for vaccinated.
1 hospitalization out of 123 cases in the unvaccinated = 0.8%; 4 hospitalizations out of 346 cases in the vaccinated = 1.2%, so the vaccinations are not reducing Delta hospitalizations.
d) In the US, government and media are blaming the spread and increase in cases on unvaccinated people, which is irrational and NOT supported by data.
The study showed that 74% of the cases (89% of cases were Delta) were in the fully vaccinated and the fully vaccinated comprised 69% of the population, which shows that the shots are not effective against Delta
(In the chart below, light blue represents fully vaccinated cases, dark blue represents not vac. - this shows that 74% of the cases are in the light blue, fully vaccinated people.)
The vaccines were designed to form antibodies against the spike protein of the original strain (alpha) only, and NOT designed to reduce transmission.
Vaccinating people with the shots designed for the old strain will NOT stop the cases of Delta and other variants that evade it, which the data is showing.
Some researchers have argued that antibody-dependent enhancement (ADE) may be occurring with the vaccines and the delta variant. This does not appear to be the case. A good overview of ADE and covid related issues to ADE are mentioned here.
https://www.chop.edu/centers-programs/vaccine-education-center/vaccine-safety/antibody-dependent-enhancement-and-vaccines
https://www.nebraskamed.com/COVID/antibody-dependent-enhancement-in-vaccines
Recent research (below) reveals that one single dose of the m-RNA vaccines appears to be very effective at preventing the severe form of covid-19 and that if you had covid-19 that the vaccine does not necessarily benefit from vaccination (see below Cleveland study and JAMA report)
The first U.S. multisite test-negative design vaccine effectiveness study among HCP found a single dose of Pfizer-BioNTech or Moderna COVID-19 vaccines to be 82% effective against symptomatic COVID-19 and 2 doses to be 94% effective.
https://www.cdc.gov/mmwr/volumes/70/wr/mm7020e2.htm
A UK study reported in the Lancet found similar results, with just one vaccine dose if measured after 15 days.
https://www.healthline.com/health/vaccinations/pfizer-vaccine-efficacy
Researchers from the Cleveland Clinic have found that people who’ve already had COVID-19 may not necessarily benefit from vaccination, according to a new small study.
They said that people with prior infection had similar protection to those who were fully vaccinated.
https://www.healthline.com/health-news/new-study-determines-people-whove-had-covid-19-dont-need-to-get-vaccinated#What-we-know-about-immunity
Study Suggests Lasting Immunity After COVID-19 (at least a year), With a Big Boost From Vaccination
https://jamanetwork.com/journals/jama/fullarticle/2782139
Vaccine after-effects more common in those who already had COVID
A third (33%) of those who had previously had COVID-19 reported at least one whole body (systemic) after effect after 7 days compared to 19% of who had not previously had COVID-19.
https://covid.joinzoe.com/post/vaccine-after-effects-more-common-in-those-who-already-had-covid
Updated information regarding the vaccines and delta variant and PCR testing:
When one wades through much of the information on Covid-19 and the PCR tests, one sees that contagion (active infection) and having had in the past covid, or been in proximity to covid-19 are being conflated.
Fauci recommends some between 30 and 35 (Ct value) has more appropriate and will produce less chance of a false positive indication of an active infection than higher values.
PCR test and Ct values (number of cycles of amplification of covid-19 specimen) (each cycle of amplification is a doubling, so a Ct value of 40 is 2 to the 40 power or 1,099,511,627,776 (more than a trillion).
"This infamous Ct value, or cycle threshold, is pretty simple. It is the number of cycles of amplification needed to get enough light. By “enough light,” we mean that it crosses the threshold where it is clearly above what would be called background noise."
Below are articles on covid and the PCR test.
“Dr. Anthony Fauci appeared to acknowledge that large numbers of positive COVID-19 cases may arise from oversensitive tests that pick up mere fragments of the virus rather than active, viable infections. If true, many patients may have been receiving false-positive test results”
https://healthfeedback.org/claimreview/claim-that-high-pcr-test-sensitivity-inflates-covid-19-cases-wrongly-conflates-the-issue-of-contagiousness-with-the-presence-of-infection/
The COVID-19 PCR Test Is Reliable Despite the Commotion About Ct Values
The people sharing the claim that COVID-19 PCR testing is not reliable because of high Ct values are just amplifying noise.
https://www.mcgill.ca/oss/article/covid-19-critical-thinking/covid-19-pcr-test-reliable-despite-commotion-about-ct-values
There is a lot of science-based information on how viruses, like covid-19, mutate to variants that are more infectious but not necessarily more deadly to raise the probability of their continued existence in a given target host like humans. The delta variant is an example of this.
The CDC keeps urging people to get vaccinated to:
1) avoid dying or filling up the ICU’s of hospitals – this appears to be a true and valid reason.
2) to create herd immunity so the virus will die out and not evolve variants.
Increasing evidence appears to make this 2nd reason less valid.
It appears the delta variant is surviving and infecting already vaccinated people, but importantly, not having the vaccinated develop a severe form of covid, the delta variant also is spreading to unvaccinated humans with a more devastating effect on the unvaccinated.
In terms of covid-19 vaccines or any vaccines an important article to read is below.
Vaccines Are Pushing Pathogens to Evolve
Just as antibiotics breed resistance in bacteria, vaccines can incite changes that enable diseases to escape their control. Researchers are working to head off the evolution of new threats.
https://www.quantamagazine.org/how-vaccines-can-drive-pathogens-to-evolve-20180510/
Clots, Strokes And Rashes. Is COVID-19 A Disease Of The Blood Vessels?
November 5, 2020
Whether it's strange rashes on the toes or blood clots in the brain, the widespread ravages of COVID-19 have increasingly led researchers to focus on how the novel coronavirus sabotages the body's blood vessels.
As scientists have come to know the disease better, they have homed in on the vascular system — the body's network of arteries, veins and capillaries, stretching more than 60,000 miles — to understand this wide-ranging disease and to find treatments that can stymie its most pernicious effects.
...
Some of the earliest insights into how COVID-19 can act like a vascular disease came from studying the aftermath of the most serious infections. Those reveal that the virus warps a critical piece of our vascular infrastructure: the single layer of cells lining the inside of every blood vessel, known as the endothelial cells or simply the endothelium.
...
It's already known that the coronavirus breaks into cells by way of a specific receptor, called ACE2, which is found all over the body. But scientists are still trying to understand how the virus sets off a cascade of events that cause so much destruction to blood vessels. Li says one theory is that the virus directly attacks endothelial cells. Lab experiments have shown that the coronavirus can infect engineered human endothelial cells.
It's also possible the problems begin elsewhere, and the endothelial cells sustain collateral damage along the way as the immune system reacts — and sometimes overreacts — to the invading virus.
Endothelial cells have a slew of important jobs; these include preventing clotting, controlling blood pressure, regulating oxidative stress and fending off pathogens. And Li says uncovering how the virus jeopardizes the endothelium may link many of COVID-19's complications: "The effects in the brain, the blood clots in the lung and elsewhere in the legs, the COVID toe, the problem with the kidneys and even the heart."
...
https://www.npr.org/sections/health-shots/2020/11/05/917317541/clots-strokes-and-rashes-is-covid-19-a-disease-of-the-blood-vessels
How mRNA Vaccine May Affect Cells
Story at-a-glance
Dr. Charles Hoffe, a family physician from Lytton, British Columbia, told health officials that his patients were suffering adverse effects from the mRNA COVID-19 vaccines
Hoffe was quickly accused of causing “vaccine hesitancy” and local health authorities threatened to report him to the licensing body
The spike protein in the vaccine can lead to the development of multiple, tiny blood clots because it becomes part of the cell wall of your vascular endothelium; these cells are supposed to be smooth so that your blood flows smoothly, but the spike protein means there are “spiky bits sticking out”
Hoffe has been conducting the D-dimer test on his patients to detect the potential presence of blood clots within four to seven days of receiving a COVID-19 vaccine; 62% have evidence of clotting
The long-term outlook is very grim, Hoffe said, because with each successive shot, it will add more damage as you’re getting more damaged capillaries
Dr. Charles Hoffe, a family physician from Lytton, British Columbia, wrote to Dr. Bonnie Henry, B.C. provincial health officer, in April 2021 with serious concerns about COVID-19 vaccines. One of his patients died after the shot, and six others had adverse effects. While their small town had no cases of COVID-19, Hoffe said the vaccine was causing serious damage and he believed “this vaccine is quite clearly more dangerous than COVID-19.”1
Hoffe was quickly accused of causing “vaccine hesitancy” and local health authorities threatened to report him to the licensing body, the College of Physicians and Surgeons of British Columbia. He was also told by government health authorities that he could not say anything negative about the COVID-19 vaccine,2 but the issues Hoffe was seeing compelled him to speak out anyway.
Blood Clot Formation With mRNA Vaccines ‘Inevitable’
Hoffe created the video above to explain how mRNA COVID-19 vaccines can affect your body at the cellular level.3 In each dose of the Moderna COVID-19 vaccine are 40 trillion mRNA — or messenger RNA — molecules.
Each mRNA “package” is designed to be absorbed into your cell, but only 25% stay in your arm at the site of the injection. The other 75%, Hoffe says, are collected by your lymphatic system and fed into your circulation. The cells where mRNA is absorbed are those around your blood vessels — the capillary network, which are the tiniest blood vessels in your body.
When the mRNA is absorbed into your vascular endothelium — the inner lining of your capillaries — the “packages” open and genes are released. Each gene can produce many COVID-19 spike proteins, and your body gets to work manufacturing these spike proteins, numbering in the trillions.
Your body recognizes the spike protein as foreign, so it begins to manufacture antibodies to protect you against COVID-19, or so the theory goes. But there’s a problem. In a coronavirus, the spike protein becomes part of the viral capsule, Hoffe says, but when you get the vaccine, “it’s not in a virus, it’s in your cells.” The spike protein, in turn, can lead to the development of blood clots:4
“So it therefore becomes part of the cell wall of your vascular endothelium, which means that these cells, which line your blood vessels, which are supposed to be smooth so that your blood flows smoothly, now have these little spiky bits sticking out.
So it is absolutely inevitable that blood clots will form, because your blood platelets circulate around in your vessels and the purpose of blood platelets is to detect a damaged vessel and block that damage when it starts bleeding. So when a platelet comes through a capillary and suddenly hits all these covid spikes that are jutting into the inside vessel … blood clots will form to block that vessel. That’s how platelets work.”
62% of Recently Vaccinated Patients Have Evidence of Clotting
Hoffe spoke with Dr. Sucharit Bhakdi, a retired professor, microbiologist and infectious disease and immunology specialist who, along with several other doctors and scientists, formed Doctors for COVID Ethics. Bhakdi has also warned that the SARS-CoV-2 spike protein binds to the ACE2 receptor on platelets.5
The subsequent activation of the platelets can lead to disseminated intravascular coagulation (DIC), i.e., a pathological overstimulation of your coagulation system that can result in abnormal, and life threatening, blood clotting, as well as thrombocytopenia (low platelet count) and hemorrhaging.
While some of the blood clots you may have heard about associated with the COVID-19 vaccines are the large variety that show up on MRIs and CT scans, Hoffe states that the variety he’s referring to are microscopic and scattered throughout the capillary network, so they won’t show up on any scan.
The only way to find out if this predictable mechanism of clotting is happening is with a test called D-dimer. D-dimer is a protein fragment produced by the body when a blood clot dissolves. It’s typically undetectable or present only at very low levels, buts its level may significantly rise when the body is forming and breaking down blood clots.6
According to Bhakdi, “Now a number of German doctors have been measuring the D-dimers in the blood of patients before vaccination and days after vaccinations and with respect to the symptoms they have just found out that triggering of clot formation is a very common event with all vaccines.”7
Hoffe has been conducting the D-dimer test on his patients within four to seven days of them receiving a COVID-19 vaccine and found that 62% have evidence of clotting.8 While he’s still trying to accumulate more information, he said:9
“It means that these blood clots are not rare. The majority of people are getting blood clots and they have no idea that they even have them. The most alarming thing about this is that there are some parts of your body, like your heart and your brain and your spinal cord and your lungs, which cannot regenerate. When those tissues are damaged by blocked vessels, they are permanently damaged.”
‘The Worst Is Yet to Come’
As Bhakdi explained, post-vaccination it’s possible to end up with so many blood clots throughout your vascular system that your coagulation system is exhausted, resulting in bleeding (hemorrhaging).10 Hoffe now has patients who get out of breath much more easily than they used to because “they’ve clogged up thousands of tiny capillaries in their lungs.” This is only the first problem, as it can lead to more significant, permanent damage. Hoffe noted:11
“The terrifying thing about this is not just that these people are short of breath and can’t do what they used to be able to do. Once you block off a significant number of blood vessels to your lungs, your heart is now pumping against a much greater resistance to try to get the blood through your lungs.”
The end result can be pulmonary artery hypertension, which is basically high blood pressure in your lungs, because the blood can’t get through due to the many vessels that are blocked. “People with this usually die of right-sided heart failure within three years,” Hoffe said. “So the huge concern about this mechanism of injury is that these shots are causing permanent damage and the worst is yet to come.”12
As he noted, while some tissues, like your liver and kidneys, can regenerate, others, like your heart, cannot. An increased risk of myocarditis, or inflammation of the heart muscle, has already been seen among young males who receive an mRNA COVID-19 vaccine.13 “They have permanently damaged hearts,” Hoffe explained, adding:14
“It doesn’t matter how mild it is, they will not be able to do what they used to do because heart muscle doesn’t regenerate. The long-term outlook is very grim, and with each successive shot, it will add more damage. The damage is cumulative because you’re progressively getting more damaged capillaries.”
Because of the risk of the formation of blood clots in your vessels, Bhakdi went so far as to say that giving the COVID-19 vaccine to children is a crime: “Do not give it to children because they have absolutely no possibility to defend themselves; if you give it to your child you are committing a crime.”15
Spike Protein Damages Human Cells
The key causative agent causing damage from COVID-19 vaccines appears to be the spike protein. Scientists from the University of California San Diego created a pseudo virus, or cell surrounded by the spike proteins that did not contain a virus.16
Using an animal model, the researchers administered the pseudo virus into the lungs and found the virus was not necessary to create damage. Instead, the spike protein was enough to cause inflammation, damage to vascular endothelial cells and inhibited mitochondrial function.
Dr. Robert Malone, the inventor of the mRNA and DNA vaccine core platform technology,17 has also spoken out about the dangers of the spike protein used in COVID-19 vaccines.
In its native form in SARS-CoV-2, the spike protein is responsible for the pathologies of the viral infection, and in its wild form it’s known to open the blood-brain barrier, cause cell damage (cytotoxicity) and, Malone said, “is active in manipulating the biology of the cells that coat the inside of your blood vessels — vascular endothelial cells, in part through its interaction with ACE2, which controls contraction in the blood vessels, blood pressure and other things.”18 Bhakdi also described this as “a disastrous situation” paving the way for clotting:19
“This is a disastrous situation, because the spike protein itself is now sitting on the surface of the cells, facing the bloodstream. It is known that these spike proteins, the moment they touch platelets, they active them [the platelets], and that sets the whole clotting system going.
The second thing that should happen, according to theory, is that the waste products of this protein that are produced in the cell, are put in front of the ‘door’ of the cell … and is presented to the immune system.
The immune system, especially the lymphocytes, recognize these and will attack the cells, because they don’t want them to make viruses or viral parts. And the viral parts are now being made in locations where viral parts would never, ever reach [naturally], like the vessel wall in your brain …
If that ‘tapestry’ of the wall [i.e., the lining of the blood vessel] is then destroyed, then that is the signal for the clotting system to [activate], and create a blood clot. And this happens with all of these vaccines because the gene [the instruction to make spike protein] is being introduced to the vessel wall.”20
Physicians Forbidden From Countering Narrative
Equally as disturbing as the potential harm caused by experimental mRNA vaccines is the censorship going along with it, such that the College of Physicians and Surgeons of Ontario (CPSO), which regulates the practice of medicine in Ontario, issued a statement21 prohibiting physicians from making comments or providing advice that goes against the official narrative — basically anything “anti-vaccine, anti-masking, anti-distancing and anti-lockdown.”22
The statement was released, according to CPSO, because physicians, in isolated incidents, have been spreading blatant misinformation via social media, which is undermining “public health measures meant to protect all of us.” But if a physician is unable to speak freely, the independent relationship between doctor and patient ceases to exist, and so does the doctor’s ability to act in the best interest of the patient.
Hoffe certainly experienced this but is still speaking out, putting his patients first and trying to get the word out that, he believes the COVID-19 vaccination program should be stopped until the causes of the many injuries and deaths are understood.23 The tragic question is, how many others with similar concerns have been intimidated into remaining silent?
https://media.mercola.com/ImageServer/Public/2021/August/PDF/how-mrna-vaccine-affects-cells-pdf.pdf
also related D-dimer increases in covid-19 patients as it does in the vaccine
D-dimer is commonly elevated in patients with COVID-19. D-dimer levels correlate with disease severity and are a reliable prognostic marker for in-hospital mortality in patients admitted for COVID-19.
https://jintensivecare.biomedcentral.com/articles/10.1186/s40560-020-00466-z
In evaluating the cost (to your health vs the benefit to your health of the covid vaccines) California statistics are useful, because it is a big diverse population state and breaks their current statistics on covid-19 into many age categories.
As of 2-2 2021
COVID-19 Cases by Age Group data as of 2-2-2002
https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/COVID-19/COVID-19-Cases-by-Age-Group.aspx
5-17 1,235,496 #of cases covid deaths 33 16.7 cases as percent of CA population
33/1235496 =.0000267 or .00267% of population or rounded .003 of every 100 people, or .03 of every 1000 or .3 of every 10,000 or 3 of every 100,000
Vaccine Adverse Event Reporting
https://wonder.cdc.gov/controller/datarequest/D8 VAERS data search
https://openvaers.com/index.php
https://openvaers.com/covid-data
https://openvaers.com/covid-data/adverse-events-by-state
5-11 total serious adverse events 724
12-18 total serious adverse events 4,068 assuming linear (581 per year) in the 7 years from 12 thru 18 then 12-17 age 3487 serious adverse events
in CA a total of 4211 serious adverse events (including death) due to covid vaccine in 5-17 age group
https://www.latimes.com/projects/california-coronavirus-cases-tracking-outbreak/covid-19-vaccines-distribution/
5-11 26+9= 35% vaccinated of 3,518,950 so 1,231,633 vaccinated
12-17 64+9 = 73% vaccinated of 3,168,617 so 2,313,090 vaccinated
https://covid19.ca.gov/vaccination-progress-data/#progress-by-group
so total of 3,544,723 vaccinated in the 5 to 17 age group in CA
so 4211/3544723 = .0012 or .12% or .12 of every 100 or 1.2 of every 1000 or 12 of every 10,000 or 120 of every 100,000
so anyone from 5 to 17 years of age has a 120/3 i.e. 40 times greater chance of a serious adverse event due to the covid vaccines than dying of covid
in contrast anyone over 65 years old has about a 200 greater chance of dying from covid compared a serious adverse event due the vaccines.
Using up to data August 4 2021
at age 50-59 6904/531177 = .0129975 or 1.3 in 100 chance of dying from covid if you get it, and are in the 50-59 age group, the chances are very similar to age bracket 50-59 for all age brackets up to 80.
Age brackets from 50 to 79, have a .0129975/.0000546 =223.32 times greater chance of dying of covid compared to age 17 and under.
The California covid statistics can be found at:
https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/COVID-19/COVID-19-Cases-by-Age-Group.aspx
Unfortunately, it appears, the US Vaccine Adverse Event Reporting System (VAERS) does not break down the data by age, but the below numbers are instructive.
https://www.openvaers.com/covid-data
https://vaers.hhs.gov/
Under reporting on VAERS
Lazarus report from Harvard Pilgrim Health Care
...
Further it states, "Adverse events from drugs and vaccines are common, but underreported. Although 25% of ambulatory patients experience an adverse drug event, less than 0.3% of all adverse drug events and 1-13% of serious events are reported to the Food and Drug Administration (FDA). Likewise, fewer than 1% of vaccine adverse events are reported."...
....
More recently Steve Kirsch and Dr. Jessica Rose have both calculated an Under Reporting Factor (URF) for Covid vaccine injuries. Steve used multiple methods to confirm a URF of approximately 41.[3] Dr. Rose used of the current Department of Defense Medical Epidemiology Database (DMED) miscarriage rates to calculate a URF of 49.[4]
https://openvaers.com/faq/what-is-underreporting-and-why-it-matters
Excel spreadsheet of VAERS and Covid Data
Study: COVID Shot Enhances Delta Infectivity?
The official COVID-19 vaccine narrative changes rapidly these days. It took just one month for it to go from “if you’re vaccinated you’re not going to get COVID,”1 including the Delta variant,2 to “people who got vaccinated early are at increased risk for severe COVID disease.”3
From the get-go, I and many other medical experts have warned of the possibility of these shots causing antibody dependent enhancement (ADE), a situation in which the shot actually facilitates a cascade of disease complications rather than protects against it. As a result, you may suffer more severe illness when encountering the wild virus than had you not been “vaccinated.”
While we don’t yet have definitive proof that ADE is occurring, we are seeing suspicious signs that it might be. Data showing those who got the shot early this year are now at increased risk of severe infection could be such a sign. At bare minimum, it’s an indication that the protection you get from these shots is very temporary, lasting only a few months.
This makes sense when you consider they program your body to produce just one type of antibody against a specific spike protein. Once the spike protein, or other elements in the virus, starts to mutate, protection radically diminishes. Worse, the vaccine facilitates the actual production of the variants because it is “leaky” and provides only partial ineffective immune protection.
Natural immunity is far superior, as when you recover from the infection, your body makes antibodies against all five proteins of the virus, plus memory T cells that remain even once antibody levels diminish. This gives you far better protection that will likely be lifelong, unless you have impaired immune function.
Real-world data from Israel confirms this, showing those who have received the COVID jab are 6.72 times more likely to get infected than people with natural immunity.4,5,6
In an August 20, 2021, report, BPR noted:7
“’The data we will publish today and next week demonstrate the vaccine effectiveness against SARS COVID 2 infection is waning,’ the CDC director [Rochelle Walensky] began … She cited reports of international colleagues, including Israel ‘suggest increased risk of severe disease amongst those vaccinated early.’
Fear not, the same people who tried to sell Americans immunity through a jab and promised to hand back the freedoms they impeded on have a plan, and they’re not leaving much room for personal choice.
‘In the context of these concerns, we are planning for Americans to receive booster shots starting next month to maximize vaccine induced protection. Our plan is to protect the American people and to stay ahead of this virus,’ Walensky shared …
The CDC director appears to all but admit that the vaccine’s efficacy rate has a strict time limit, and its protections are limited in the ever-changing environment.
‘Given this body of evidence, we are concerned that the current strong protection against severe infection, hospitalization and death could decrease in the months ahead. Especially among those who are higher risk or those who were vaccinated earlier during the phases of our vaccination roll out,’ Walensky explained …
Starting September 20, Americans who completed their two doses of the Pfizer or Moderna vaccine at least eight months ago will be eligible for a booster shot. The goalposts back to a ‘normal’ society continue to be moved further and further. When will Americans, especially those who complied with initial vaccinations, have had enough?”
Indeed, Israeli data show Pfizer’s shot went from a 95% effectiveness at the outset, to 64% in early July 2021 and 39% by late July, when the Delta strain became predominant.8,9 Meanwhile, the U.S. Food and Drug Administration’s expectation for any vaccine is an efficacy rate of at least 50%.
Pfizer’s own trial data even showed rapidly waning effectiveness as early as March 13, 2021. BMJ associate editor Peter Doshi discussed this in an August 23, 2021, blog.10
By the fifth month into the trial, efficacy had dropped from 96% to 84%, and this drop could not be due to the emergence of the Delta variant since 77% of trial participants were in the U.S., where the Delta variant didn’t emerge until months later. This suggests the COVID shot has a very temporary effectiveness regardless of new variants.
What’s more, while Israeli authorities claim the Pfizer shot is still effective at preventing hospitalization and death, many who are double-jabbed do end up in the hospital, and we’re already seeing a shift in hospitalization rates from the unvaccinated to those who have gotten one or two injections. For example, by mid-August, 59% of serious COVID cases were among Israelis who had received two COVID injections.11
Data from the U.K. show a similar trend among those over the age of 50. In this age group, partially and fully “vaccinated” people account for 68% of hospitalizations and 70% of COVID deaths.12

Data13 from the U.S. Centers for Disease Control and Prevention also raise questions about the usefulness of the COVID shots. Between July 6 and July 25, 2021, 469 COVID cases were identified in a Barnstable County, Massachusetts, outbreak.
Of those who tested positive, 74% had received two COVID injections and were considered “fully vaccinated.” Even despite using different diagnostic standards for non-jabbed and jabbed individuals, a whopping 80% of COVID-related hospitalizations were also in this group.14,15
Although Pfizer-BioNTech BNT162b2-immune sera neutralized the Delta variant, when four common mutations were introduced into the receptor binding domain (RBD) of the Delta variant (Delta 4+), some BNT162b2-immune sera lost neutralizing activity and enhanced the infectivity. ~ bioRxiv, August 23, 2021
The CDC also confirmed that fully vaccinated individuals who contract the infection have as high a viral load in their nasal passages as unvaccinated individuals who get infected, proving there’s no difference between the two, in terms of being a transmission risk.16
If vaccination status has no bearing on the potential risk you pose to others, why do we need vaccine passports? According to Harvard epidemiologist Martin Kulldorff, this evidence demolishes the case for passports.17 They clearly cannot ensure safety, as evidenced by outbreaks where the vaccination rate was 100%. Examples include outbreaks onboard a Carnival cruise liner18 and the HMS Queen Elizabeth, a British Navy flagship.19
A study20 posted August 23, 2021, on the preprint server bioRxiv now warns the Delta variant “is posed to acquire complete resistance to wild-type spike vaccines.” This could essentially turn into a worst-case scenario that sets up those who have received the Pfizer shots for more severe illness when exposed to the virus. As explained by the authors:21
“Although Pfizer-BioNTech BNT162b2-immune sera neutralized the Delta variant, when four common mutations were introduced into the receptor binding domain (RBD) of the Delta variant (Delta 4+), some BNT162b2-immune sera lost neutralizing activity and enhanced the infectivity.
Unique mutations in the Delta NTD were involved in the enhanced infectivity by the BNT162b2-immune sera. Sera of mice immunized by Delta spike, but not wild-type spike, consistently neutralized the Delta 4+ variant without enhancing infectivity.
Given the fact that a Delta variant with three similar RBD mutations has already emerged according to the GISAID database, it is necessary to develop vaccines that protect against such complete breakthrough variants.”
It’s now clear that early warnings against mass vaccination during an active outbreak are being realized. It’s not the unvaccinated that are driving mutations; it’s the vaccinated, as the injections simply do not prevent infection.
The end result, if we keep going, will be a treadmill of continuous injections to keep up with the merry-go-round of waning effectiveness in general combined with the emergence of vaccine-resistant variants. As reported by Live Science:22
“Vaccine-resistant coronavirus mutants are more likely to emerge when a large fraction of the population is vaccinated and viral transmission is high … In other words, a situation that looks a lot like the current one in the U.S.
The mathematical model,23 published July 30 in the journal Scientific Reports, simulates how the rate of vaccination and rate of viral transmission in a given population influence which SARS-CoV-2 variants come to dominate the viral landscape …
If viral transmission is low, any vaccine-resistant mutants that do emerge get fewer chances to spread, and thus, they're more likely to die out, said senior author Fyodor Kondrashov, who runs an evolutionary genomics lab at the Institute of Science and Technology Austria.”
These findings come as no surprise to those familiar with previous research showing the same exact thing. As explained in “Vaccines Are Pushing Pathogens to Evolve,” published in Quanta Magazine,24 “Just as antibiotics breed resistance in bacteria, vaccines can incite changes that enable diseases to escape their control.”
The article details the history of the anti-Marek’s disease vaccine for chickens, first introduced in 1970. Today, we’re on the third version of this vaccine, as within a decade, it stops working. The reason? The virus has mutated to evade the vaccine. As a result of these leaky vaccines, the virus is becoming increasingly deadly and more difficult to treat.
A 2015 paper25 in PLOS Biology tested the theory that vaccines are driving the mutation of the herpesvirus causing Marek’s disease in chickens. To do that, they vaccinated 100 chickens and kept 100 unvaccinated. All of the birds were then infected with varying strains of the virus. Some strains were more virulent and dangerous than others.
Over the course of the birds’ lives, the unvaccinated ones shed more of the least virulent strains into the environment, while the vaccinated ones shed more of the most virulent strains. As noted in the Quanta Magazine article:26
“The findings suggest that the Marek’s vaccine encourages more dangerous viruses to proliferate. This increased virulence might then give the viruses the means to overcome birds’ vaccine-primed immune responses and sicken vaccinated flocks.”
Before 2021, it was quite clear that vaccines push viruses to mutate into more dangerous strains. The only question was, to what extent? Now all of a sudden, we’re to believe conventional science has been wrong all along. Here’s another example: NPR as recently as February 9, 2021, reported that “vaccines can contribute to virus mutations.” NPR science correspondent Richard Harris noted:27
“You may have heard that bacteria can develop resistance to antibiotics and, in a worst-case scenario, render the drugs useless. Something similar can also happen with vaccines, though, with less serious consequences.
This worry has arisen mostly in the debate over whether to delay a second vaccine shot so more people can get the first shot quickly. Paul Bieniasz, a Howard Hughes investigator at the Rockefeller University, says that gap would leave people with only partial immunity for longer than necessary.”
According to Bieniasz, partially vaccinated individuals “might serve as sort of a breeding ground for the virus to acquire new mutations.” This is the exact claim now being attributed to unvaccinated people by those who don’t understand natural selection.
It’s important to realize that viruses mutate continuously and if you don’t have a sterilizing vaccine that blocks infection completely, then the virus mutates to evade the immune response within that person. That is one of the distinct features of the COVID shots — they’re not designed to block infection. They allow infection to occur and at best lessen the symptoms of that infection. As noted by Harris:28
“This evolutionary pressure is present for any vaccine that doesn't completely block infection … Many vaccines, apparently, including the COVID vaccines, do not completely prevent a virus from multiplying inside someone even though these vaccines do prevent serious illness.”
In short, like bacteria mutate and get stronger to survive the assault of antibacterial agents, viruses can mutate in vaccinated individuals who contract the virus, and in those, it will mutate to evade the immune system.
In an unvaccinated person, on the other hand, the virus does not encounter the same evolutionary pressure to mutate into something stronger. So, if SARS-CoV-2 does end up mutating into more lethal strains, then mass vaccination is the most likely driver.
As reported August 27, 2021, by MSN,29 as players were encouraged to get the COVID shot for everyone’s safety, separate testing rules were put into place. Players who have gotten the jab only need to test every two weeks, while unvaccinated players undergo daily testing.
The relaxed testing requirement for double-jabbed players was used as incentive to go ahead and get the shot. As reported by MSN, “Conversely, the continued daily testing would become part of a punitive system that would make life so annoying for the unvaccinated that they would eventually get on board.”30
Well, this didn’t work out as planned. Nine Titans players and head coach Mike Vrabel have now tested positive, showing it really doesn’t matter if you’re double-jabbed or not. The infection spreads among the vaxxed just the same. As noted by MSN:31
“The pandemic is in a phase where the unvaccinated are facing the vengeance of a more aggressive strain of COVID-19. It's also an era when the vaccinated are grappling with the reality that their shots are mitigating their symptoms and medical complications, but not completely preventing them from becoming infected or transmitting COVID to others.”
To remedy the matter, the NFL Players Association, the union representing players of the National Football League, is now calling for a return to daily testing of all players, regardless of COVID jab status. Time and again, we find that incentives fall far short of their initial promise. This has been the case for masks as well.
First, we were told that if we got the COVID shot, we didn’t need to wear masks anymore. Of course, universal mask recommendations returned full force when it became apparent that breakthrough infections were still occurring at a surprising rate.
Now, routine testing with a test known to produce false positives at a rate of about 97%32 is promoted again, regardless of injection status, and there’s no reason to assume the same won’t happen with vaccine passports. We’re promised freedom if we give up medical autonomy, but freedom will never actually be granted. They’ll just continue to move the goal post.
It is highly likely, in fact even predictable, that despite its dramatic ineffectiveness, the requirement for one or two COVID jabs will soon be turned into three, and vaccine passport holders who don’t want to get that third shot will be back at Square 1. They’ll be just as undesirable as those who got no shots.
Considering the speed at which SARS-CoV-2 is mutating, you can be assured there’ll be a fourth shot, and a fifth and, well, you get the idea. Vaccine passports and COVID jab requirements will simply lead to a situation where you have to keep getting additional shots or lose all your privileges.
Of course, every single injection comes with health risks, and the risk for an adverse event will probably get bigger and bigger with each additional shot, and you don’t need to be a modern-day Nostradamus to see where this will lead us.
Unfortunately, rather than accepting reality — which is that SARS-CoV-2 is here to stay, just like any number of other common cold and influenza viruses — and stopping the merry-go-round of injections that only make matters worse, President Biden said he’d spoken with Dr. Anthony Fauci about giving booster shots at the five-month mark after the initial round of injections rather than waiting eight months, as previously suggested.33
While Fauci quickly responded34 that eight months was still the goal, he also said that “we are open to data as they come in” if the Food and Drug Administration and the Advisory Committee on Immunization Practices determine a sooner timeline is necessary.
Israel began administering a third booster shot to people over the age of 60 July 30, 2021. August 19, eligibility for a booster was expanded to include people over the age of 40, as well as pregnant women, teachers and health care workers, even if they’re younger than 40. Initial reports suggest the third dose has improved protection in the over-60 group, compared to those who only got two doses of Pfizer.35 According to Reuters:36
“Breaking down statistics from Israel's Gertner Institute and KI Institute, ministry officials said that among people aged 60 and over, the protection against infection provided from 10 days after a third dose was four times higher than after two doses. A third jab for over 60-year-olds offered five to six times greater protection after 10 days with regard to serious illness and hospitalization.”
Anyone who thinks one or more booster shots are the answer to SARS-CoV-2 is likely fooling themselves though. I look forward with trepidation to data on hospitalization and death rates, not to mention side effect rates, in the months to come.
Knowing what we already know about the risks of these shots and their tendency to encourage mutations, it seems reasonable to suspect that all we’re doing is digging ourselves an ever-deeper, ever-wider hole that’s going to be increasingly difficult to get out of.
Masks update
If one wades through the CDC article below, especially the charts, one sees that a person (not in a restaurant) has a 1.8 % increased chance of not testing positive for covid-19 and 1.9% chance of dying from covid-19, by wearing a mask.
If in a restaurant (many consider at near worst case situation) then your chances of not testing positive are bettered by the mask by 1.1%, and not dying from covid-19 are improved by 3%.
In both cases the best outcomes are at 81 to 100 days. see paper below in link
https://www.cdc.gov/mmwr/volumes/70/wr/pdfs/mm7010e3-H.pdf
Effectiveness of Mask Wearing to Control Community Spread of SARS-CoV-2
https://jamanetwork.com/journals/jama/fullarticle/2776536
Among our 7324 identified cases in China with sufficient descriptions, only one outdoor outbreak involving two cases
https://www.sciencemediacentre.org/expert-comments-about-outdoor-transmission-of-sars-cov-2-and-use-of-facemasks-outdoors/
In Summary, wearing a mask indoors in a public place gives one a small but statistically significant advantage in avoid covid-19.
Wearing a mask outdoors, when you are sure you can be at least 6 feet from other individuals is a disadvantage to one’s health. Among other things this can be measured by using a pulse oximeter to measure one’s pulse and oxygen level with Mask on and Mask off.
Ivermectin
Is Ivermectin a safe way to fight COVID-19 as Delta-variant cases rise?
https://www.clarkcountytoday.com/news/is-ivermectin-a-safe-way-to-fight-covid-19-as-delta-variant-cases-rise/
Table 2c. Ivermectin: Selected Clinical Data
Last Updated: July 19, 2021
The Panel has reviewed other clinical studies of IVM for the treatment of COVID-19.1-16 However, those studies have limitations that make them less definitive and informative than the studies discussed here. The studies summarized below are those that have had the greatest impact on the Panel’s recommendations.
https://www.covid19treatmentguidelines.nih.gov/tables/table-2c/
Part 1:
In viewing some of the information on this webpage, it is good to keep in mind that many biological processes operate on a probability curve, binary answers (yes or no) tend to be over-simplifications that the general public wants. This aspect of biology shows up in tests for infection diseases like covid-19, for both the antibodies tests and the PCR tests for the virus itself. Generally, it is helpful to remember, duration of exposer + quantity of virus + immune system state are important variables for infectious diseases.
It helps to understand that, with a small percent of exceptions, the immune system of a person age 30 and under, has a rapid and stronger response at producing antibodies to a novel infectious agent like covid-19 than the same person when they are over 65 years old.
The basics of the progression of the covid-19 virus in an infected individual, is somewhat atypical of many viral infections.
How long does it take for symptoms of COVID-19 to appear?
Symptoms of COVID-19 typically appear 2–14 days after exposure to the virus, and the mean incubation period is 5.1 days. The findings of 2020 research on 181 confirmed cases of SARS-CoV-2 infection suggest that 97.5% of those who are symptomatic will begin to show symptoms within 11.5 days.
Typical/atypical covid-19 progression for people, who exhibit symptoms:
1) A person is infected with the covid-19 virus.
2) 2 to 14 days, median time 5 days, they start showing symptoms of the disease: sore throat, fever, chills, dry cough, sometimes stomach and gut related problems like nausea and diarrhea, loss of smell, profound tiredness.
Teenagers and young adults in some cases have developed painful red and purple lesions on the fingers and toes, but few other serious symptoms.
3) The above symptoms typically last 7 to 14 days, during this time there are usually improvements and the individual may feel they are getting over the disease.
4) Then the 2nd stage of the disease can take place, typically starting in days 8 to 14, if the person’s immune system as not created enough antibodies to quell the infection. The symptoms of this stage can be similar to stage 1 with the addition of lowered blood oxygen, below 94% using spO2 measurement (hypoxia), and some difficulty breathing, but the person’s x-ray of their lungs may show little to no pneumonia at the very start of stage 2. A CT-Scan may show some abnormalities.
5) If this lower oxygen blood measurement continues, and starts declining (sometimes rapidly) organs such as lungs, heart, kidneys become damaged and this promotes the immune system to start a cytokine storm and a hyper-inflammatory reaction that then fills up the lungs with exudate.
In individuals with good immune systems (typically younger individuals) step 4 and step 5 may not happen, because their system has produced enough antibodies to the virus to lower the viral load.
Normal Chest X-ray Doesn't Rule Out COVID-19
In brief, radiologists were asked to reread x-rays of known covid-19 patients, and most in the early stages of the infection had what appeared to be normal lung x-rays.
Upon second inspection, 371 (58.3%) of the 636 chest X-rays were classified as normal. Of the 265 (41.7%) re-read as abnormal, 195 were classified as mild disease, 65 as moderate, and 5 as severe. That is, 89% (566 of 636) of the scans were re-read as normal or mildly abnormal.
https://www.webmd.com/lung/news/20200417/normal-chest-x-ray-doesnt-rule-out-covid-19#1
This subsection of Part 1 shows what happens in the ER and ICU and how that may need to change for a better patient outcome.
In the ICU, besides saved lives, this is where deaths and/or long term body damage occurs, partly due to the current treatment protocol.
This short (6 minutes) video by an Emergency Room and ICU, MD (Cameron Kyle-Sidell) in New York, illuminates the conundrum of emergency room and ICU treatment of covid-19, and sets the stage for the possible answers provided on this webpage starting with "ICU change of protocol to less harmful methods".
https://www.youtube.com/watch?v=k9GYTc53r2o
Update:
The above video seems to have started a reexamination of the ICU protocol, which includes oxygen, plus assisted breathing, intubation/ventilation, administered to covid-19 patients. We will see how long this less harmful protocol involving less use of ventilators, takes to ripple through the world, now that it is echoed and amplified in prominent publications.
Do COVID-19 Vent Protocols Need a Second Look?
John Whyte, MD, MPH; Cameron Kyle-Sidell, MD
https://www.medscape.com/viewarticle/928156
What You Should Know Before You Need a Ventilator - (from a professor of Medicine addressing the downsides of ventilators)
https://www.nytimes.com/2020/04/04/opinion/coronavirus-ventilators.html
ICU change of protocol to less harmful methods:
Partly, as a consequence of the initial video by Kyle-Sidell, MD, a prominent MD in Europe has written an article in two respected medical journals advocating in some detail how the current protocol (as of 4-13-20) needs to change (see below).
Is protocol-driven COVID-19 respiratory therapy doing more harm than good?
This article by a Professor MD explains in some detail how the current protocol might be adjusted given the hypoxia is the starting point of the chain of severe events.
https://www.the-hospitalist.org/hospitalist/article/220301/coronavirus-updates/protocol-driven-covid-19-respiratory-therapy-doing
COVID-19 Hypoxemia: A Better and Still Safe Way
Written by Salim Rezaie REBEL Covid-19, REBEL EM Medical Category: Infectious Disease, Resuscitation
https://rebelem.com/covid-19-hypoxemia-a-better-and-still-safe-way/
UChicago Medicine doctors see 'truly remarkable' success using ventilator alternatives to treat COVID-19
Doctors at the University of Chicago Medicine are seeing “truly remarkable” results using high-flow nasal cannulas rather than ventilators and intubation to treat some COVID-19 patients.
High-flow nasal cannulas, or HFNCs, are non-invasive nasal prongs that sit below the nostrils and blow large volumes of warm, humidified oxygen into the nose and lungs. ...
see complete article at following link.
https://www.uchicagomedicine.org/forefront/coronavirus-disease-covid-19/uchicago-medicine-doctors-see-truly-remarkable-success-using-ventilator-alternatives-to-treat-covid19
The above is in bold because it is so important, if you end up with the severe form of covid-19 to have an ICU that embraces this technique before using a ventilator.
If you follow the thread on the reddit link below you will gain even more of understanding of what the HFNC method for covid-19 means. In brief:
"HFNC offers several advantages compared to conventional oxygen therapy, including:
Ability to deliver O2 at up to 60 LPMs at nearly 100% FiO2. This is huge compared to regular Nasal Cannula (1-6 LPMs, maxing out at 45% FiO2) and NRB (10-15 LPMs, ~ 95% FiO2)."
https://www.reddit.com/r/COVID19/comments/g7kr1o/uchicago_medicine_doctors_see_truly_remarkable/
You normally breath in about 8 liters of air per minute (LPM), which is 21% oxygen.
Part of the technique to increase oxygenation in covid-19 patients
Coronavirus patients are being flipped onto their stomachs in the ICU — here’s why
https://globalnews.ca/news/6788251/breathing-technique-coronavirus/
Prone position in acute respiratory distress syndrome
Science study on
https://erj.ersjournals.com/content/20/4/1017
Since Oxygen Therapy may be an important part of avoiding intubation/ventilation, below link is an easy to understand look at oxygen therapy in general.
https://www.houstonlungdocs.com/oxygen-therapy/
Fact check on the part misinformation, that higher medicare payment for covid-19 is driving the reporting and over-use of ventilators:
Hospitals get paid more if patients and listed as COVID-19, on ventilators
Misstatement:
1) "if they're Medicare – typically, the diagnosis-related group lump sum payment would be $5,000. But if it's COVID-19 pneumonia, then it's $13,000, and if that COVID-19 pneumonia patient ends up on a ventilator, it goes up to $39,000."
Accurate add-on amount:
"coronavirus relief legislation created a 20% premium, or add-on, for COVID-19 Medicare patients.", which normally is less then the above amounts.
2)...may pressure physicians to cite all diagnoses, including "probable" COVID-19, on discharge papers or death certificates to get the higher Medicare allocation allowed under the Coronavirus Aid, Relief and Economic Security Act.
More Accurate Statement:
This could be happening in states that do not require laboratory verified covid-19 diagnosis, like New York.
In states like California and Minnesota this less likely to happen given these states list only laboratory-confirmed COVID-19 diagnoses
https://www.usatoday.com/story/news/factcheck/2020/04/24/fact-check-medicare-hospitals-paid-more-covid-19-patients-coronavirus/3000638001/
A summary of three different theories of how covid-19 affects the body in severe cases and how this affects the ICU (Intensive Care Unit) treatment of patients.
The current protocol, in many hospitals, for covid-19 assumes the virus is directly damaging lung tissue and the hyper-inflammatory reaction (sepsis) preceded by a cytokine storm that occurs in late stage severe convid-19 is due to that direct damage.
A theory shows how there is evidence the virus might be causing extreme hypoxia (lack of oxygen) and death, by viral proteins that are interfering with hemoglobin's role in oxygen transport, and this occurs before the cytokine storm and the destruction of the lungs and other organs. In other words, the hypoxia starts the destruction of the lungs and other organs, which then starts the cytokine storm and hyper-inflammatory reaction that then fills up the lungs with exudate.
This theory has been recently challenged, both side are presented in this web page.
Treatment using the current ICU protocol are stepped through in detail, and proposed changes based on the theory that hypoxia due to the virus interfering with hemoglobin is outlined.
A newer theory also related to the virus and blood is that the new coronavirus is invading endothelial cells.
What explains the non-respiratory symptoms seen in some COVID-19 patients?
Some patients experience neurological, cardiovascular, and intestinal symptoms after infection with SARS-CoV-2
by Megha Satyanarayana
April 14, 2020
https://cen.acs.org/biological-chemistry/infectious-disease/What-explains-non-respiratory-symptoms-seen-in-some-COVID-19-patients/98/web/2020/04
Six months of coronavirus: the mysteries scientists are still racing to solve
From immunity to the role of genetics, Nature looks at five pressing questions about COVID-19 that researchers are tackling.
03 July 2020
Six months of coronavirus: the mysteries scientists are still racing to solve
From immunity to the role of genetics, Nature looks at five pressing questions about COVID-19 that researchers are tackling.
https://www.nature.com/articles/d41586-020-01989-z
How COVID Kills Some People But Not Others - I'm a Lung Doctor (MEDICAL TRUTH)
As goes through the details about how covid-19 enters the body and steps through the destruction in severe cases
22 minutes
https://www.youtube.com/watch?v=LV8wWhjTKRU
Part 2:
Relevant statistics to Covid-19 and the ICU
In the USA the CDC (Center for Disease Control) age divisions are of greater age range than equivalent agencies in many other countries, since this website is USA based, whenever possible the CDC data is used.
As of March 22, 2020
CDC claims there had been no ICU admits or deaths reported among people under age 20 as of 3-22-20
CDC covers a huge 20-44 age range in its data, 14.3 percent hospitalized, 2 percent in the ICU, and 0.1 percent died
45 to 54, the CDC reports 21.2 percent have been hospitalized, 5.4 percent in the ICU, and 0.5 percent have died.
55 to 64, 20.5 percent have been hospitalized, 4.7 percent ended up in the ICU, and 1.4 percent died.
65 to 74, hospitalizations (28.6 percent), ICU stays (8.1 percent) and deaths (2.7 percent)
75 to 84, hospitalizations (30.5 percent), ICU stays (10.5 percent), and deaths (4.3 percent)
85 and older; 31.3 percent hospitalized, 6.3 percent in the ICU, 10.4 percent fatality rate.
From: https://www.vox.com/2020/3/23/21190033/coronavirus-covid-19-deaths-by-age
(on the above website besides CDC data, see other countries data, which in some cases shows a smaller age range in their divisions)
April 8, 2020 The Post did a state by state after the above data, which sheds some light on the younger cohorts.
"The risk appears to rise with every decade of age. The Post found at least 45 deaths among people in their 20s, at least 190 deaths among people in their 30s, and at least 413 deaths among people in their 40s."
https://www.washingtonpost.com/health/2020/04/08/young-people-coronavirus-deaths/
With an overall admission rate of covid-19 patients to the ICU being approximately 5% in the USA and the UK,
The reported mortality rate is 48% , and 66% if a ventilator is used.
It also appears an almost 100% lung and/or other organ damage rate for Covid-19 patients, who have had to have ventilation and survived.
Worldwide 86% of convid-19 patients, who go on a ventilator die (see part 3 on this webpage).
As of June 24, 14.5 deaths per 100,000 people in California overall , (.0145%).
Details of tests to detect covid-19 and tests to detect antibodies to covid-19
A good short video tutorial (27 mintues) on the state of covid-19 diagnostic testing, as of May 28, 2020, can be found at:
https://www.youtube.com/watch?v=ajiLSwJLqSk
The testing segment starts 1 hour and 6 minutes into the total video of:
UCSF School of Medicine, Medical Grand Rounds presentation.
The covid-19 testing segment presented by:
Chaz Langelier, MD PhD, UCSF Asst. Professor Division of Infectious Diseases
Includes how different tests compare, plus stage of infection plus how long shedding of virus (infectious stage when virus can still be cultured) etc.
A very brief summary of some of the video segments main points (plus some from other information):
Currently the Gold Standard is RT-PCR covid-19 which targets 2 genes
a study of the system shows the following accuracy: 1 test 88.6%, 2 test 95.7% 3 test 100%
A study presented shows that 8 days after covid-19 symptoms start that the virus can no longer be cultured, which means that it is a low probability that the patient can infect others. A cautious criteria is used by:
"World Health Organization and the Centers for Disease Control and Prevention estimate that people can be considered recovered and non-infectious 10 days after their symptoms began, as long as they have been symptom-free for three days."
The RT- PCR test is so sensitive that it can pick-up covid-19 RNA up to 55 days (rare), even in patients whose symptoms have stopped and their infectious period has passed.
A time to test for the appearance of covid-19 antibodies is at least 10 days (20 days better) after the start of symptoms.
Studies show that the FDA approved home kit for either salvia or nasal swap test for covid-19 are equally accurate, currently (as of 6-17-20) available by prescription only. Also there is a home kit an antibody test available by prescription only.
How to Fix COVID-19 Testing Q/A with Dr. Michael Mina: Cheap, At Home, Rapid Antigen Tests
Dr. Michael Mina, MD, Ph.D from the Harvard T.H Chan School of Public Health answer questions about how cheap (approx. $1), at-home, COVID-19 tests (results in 15 minutes) could be utilized to dramatically slow the spread of this pandemic (and open up schools etc. in a faster and safer way).
Dr. Mina's research has shown that the sensitivity of these simple saliva paper antigen tests (the technology already exists) is high enough to detect the vast majority of infectious COVID-19 and could be utilized frequently at home.
He also discusses the FDA regulatory problem that prevents these tests from being available now.
https://www.youtube.com/watch?v=3seIAs-73G8&feature=youtu.be
Virological assessment of hospitalized patients with COVID-2019
Roman Wölfel, et al
https://www.nature.com/articles/s41586-020-2196-x
Criteria for releasing COVID-19 patients from isolation
Patients without symptoms -- 10 days
Patients with symptoms - 14 days
https://www.who.int/news-room/commentaries/detail/criteria-for-releasing-covid-19-patients-from-isolation
Predicting infectious SARS-CoV-2 from diagnostic samples
Jared Bullard, MD
https://academic.oup.com/cid/article/doi/10.1093/cid/ciaa638/5842165
Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January-March 2020: retrospective cohort study - BMJ
Shufa Zheng et al
To evaluate viral loads at different stages of disease progression in patients infected with the 2019 severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) during the first four months of the epidemic in Zhejiang province, China.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7190077/
Symptom-Based Strategy to Discontinue Isolation for Persons with COVID-19
https://www.cdc.gov/coronavirus/2019-ncov/community/strategy-discontinue-isolation.html
A recent study from the Korean Centers for Disease Control and Prevention tracked 285 COVID-19 survivors who had tested positive for the coronavirus after their illness had apparently resolved, as indicated by a previous negative test result. The virus samples collected from them couldn’t be grown in culture, indicating the patients were shedding non-infectious or dead virus particles.
https://www.npr.org/sections/goatsandsoda/2020/05/22/861061727/south-korean-study-shows-no-evidence-recovered-covid-patients-can-infect-others
The COVID-19 RT-PCR Test: How to Mislead All Humanity. Using a “Test” To Lock Down Society
By Dr. Pascal Sacré
Global Research, November 28, 2020
https://www.globalresearch.ca/covid-19-rt-pcr-how-to-mislead-all-humanity-using-a-test-to-lock-down-society/5728483
Study that shows COVID-19 antibodies rapidly decline has many concerned
These data suggest that asymptomatic individuals had a weaker immune response to SARS-CoV-2 infection. The reduction in IgG and neutralizing antibody levels in the early convalescent phase might have implications for immunity strategy and serological surveys.
https://www.dailykos.com/stories/2020/6/24/1955596/-Widely-cited-study-has-left-some-doubting-a-COVID-19-vaccine-is-possible-but-not-so-fast
Also, orginal article in a science journal
https://www.nature.com/articles/s41591-020-0965-6
Scientists See Signs of Lasting Immunity to Covid-19, Even After Mild Infections
New research indicates that human immune system cells are storing information about the coronavirus so they can fight it off again.
By Katherine J. Wu
Published Aug. 16, 2020 Updated Aug. 17, 2020
To the immune system, not all germs are equally memorable. But our body’s cells seem to be seriously studying up on the coronavirus.
Scientists who have been monitoring immune responses to the virus are now starting to see encouraging signs of strong, lasting immunity, even in people who developed only mild symptoms of Covid-19, a flurry of new studies suggests. Disease-fighting antibodies, as well as immune cells called B cells and T cells that are capable of recognizing the virus, appear to persist months after infections have resolved — an encouraging echo of the body’s enduring response to other viruses.
...
https://www.nytimes.com/2020/08/16/health/coronavirus-immunity-antibodies.html
Hosptial Blood chemistry test results for covid-19 patients with active symptoms:
...
WBC low, Lymphocytes low, platelets lower then their normal, Procalcitonin normal in 95% CRP and Ferritin elevated most often. CPK, D-Dimer, LDH, Alk Phos/AST/ALT commonly elevated.
Basically, if you have a bilateral pneumonia with normal to low WBC, lymphopenia, normal procalcitonin, elevated CRP and ferritin- you have covid-19 and do not need a nasal swab to tell you that. A ratio of absolute neutrophil count to absolute lymphocyte count greater than 3.5 may be the highest predictor of poor outcome.
An elevated Interleukin-6 (IL6) is an indicator of their cytokine storm. If this is elevated watch these patients closely with both eyes.
Other factors that appear to be predictive of poor outcomes are thrombocytopenia and LFTs 5x upper limit of normal...
The above is extracted From Part 3 of this webpage
Leukoerythroblastic reactions in blood usually indicate a significant deviation to the body’s normal immune response. They resemble immature red blood cells (RBCs) and bone marrow cells (myeloid cells) circulating in the blood.
Upon admission, the patient’s initial blood tests revealed a normal white blood cell (WBC) count, reduced level of lymphocytes (one type of WBCs), insufficient normal-sized RBCs and a normal platelet count. Three days later, the patient had an increased level of WBCs (leukocytosis) and above normal levels of immature neutrophil cells. Her blood test also showed a mild increase in the number of monocytes (immune cells) and a reduced level of lymphocytes.
The leukoerythroblastic picture reflected normal shaped and sized RBCs but in lower than normal levels (normocytic anemia), occasional immature RBCs (nucleated), a mild presence of RBCs with different sizes (anisocytosis) and rare tear-drop shaped cells known as dacrocytes. It also showed neutrophilia, highlighting the body’s rush to produce WBCs to fight the infection.
As the patient got better, the neutrophilia resolved, and the other blood indicators were back to normal ranges. The patient has since been discharged and is recovering at home.
https://health.ucdavis.edu/health-news/newsroom/what-the-blood-tests-of-a-covid-19-patient-can-tell-us/2020/03
Leukoerythroblastic reaction in a patient with COVID-19 infection
Leukoerythroblastic reactions, defined as immature erythroid and immature myeloid cells circulating in the peripheral blood, are uncommon. Leukoerythroblastic blood findings are typically seen in disorders.
associated with bone marrow fibrosis including myelofibrosis and other myeloproliferative disorders, and cancers with metastatic disease to the bone marrow. Leukoerythroblastosis can rarely be seen in viral infections such as parvovirus [1,2]
http://www.sah.org.ar/pdf/covid-19/ajh_25793.pdf
Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study
https://www.nature.com/articles/s41392-020-0148-4
When will it be over:
Two answers plus illustrations plus quick R zero and herd immunity tutorial.
Video with some of the information from this section of the website.
https://youtu.be/uWHV8HDsZPc
Can be answered on two levels:
The first level is when the phased reopening starts on a state by state basis using CDC guide lines. Using this criteria: is when the Mortality Rate (CMR - Crude Mortality Rate) (CDR - crude death rate) drops below .3 per million, that is, at daily death rate due to covid-19 of less than 300 per 100,000 of State population. This occurred on April 27, 2020 in California, according to the website below. The phased reopening takes place over 90 days with increasing activities allowed each 30 days.
From June 8, 2020
"Forecasting when the Coronavrius outbreak will end is difficult. First because "end" as a definition is not clearly defined. Here, we will use the (policy) definition - when the daily death rate drops below 0.3 per million - as the indicator of the end of this pandemic in individual state. ...
for California this was: May 13, 2020
...Prediction programs estimate that the spread of COVID-19 on a global scale will end by December 2020; however, with the implementation of social distancing, wearing masks, and antibody/PCR tests, the United States will begin functioning again before there is a vaccine.
Per the reopening guidelines, there will be 3 phases which could last up to 30 days each. This means social distancing, contact tracing, and other public health measures will last up to 2-3 months post peak dates."
https://www.talktomira.com/post/when-will-coronavirus-peak-and-end-social-distancing
As of June 24, 14.5 deaths per 100,000 people in California overall , (.0145%).
Forecasting the impact of the first wave of the COVID-19 1 pandemic on hospital demand and deaths for the USA and 2 European Economic Area countries 3 IHME COVID-19 health service utilization forecasting team
https://www.medrxiv.org/content/10.1101/2020.04.21.20074732v1.full.pdf
Coronavirus (COVID-19) Mortality Rate (CMR - Crude Mortality Rate) (CDR - crude death rate)
Last updated: May 14, 22:00 GMT
https://www.worldometers.info/coronavirus/coronavirus-death-rate/
The 2nd level of an answer to: When will it be over? Is the herd immunity related answer:
As of December 2021, The below percents are likely wrong but the discussion and examples of Herd Immunity still hold.
See current projections at the end of the below tutorial on herd immunity and endemic.
When 50% to 70% of Americans are infected and develop antibodies to covid-19, that is, herd immunity will occur at that point. Covid-19 will go from being an Epidemic (spreading) to Endemic (stable not spreading) in the US.
This is based on an infectious rate for covid-19 (R0)(R zero) for a given individual infecting 2 to 2.5 other people on average. The equation epidemiologist use is 1 - 1/R0, so if R0 equals 2, than 1-(1/2) = .5 or 50%. It should be understood that the value of R0 varies from place to place. It is also based on how infectious the stain of the virus is.
In highly dense places, where social distancing is not possible, the value of R0 might be something like 5 for the current stain of covid-19, than it follows that 1-(1/5)= .8 or 80% of that population must have to have developed antibodies to covid-19 to reach herd immunity.
The World Is Still Far From Herd Immunity for Coronavirus
By Nadja Popovich and Margot Sanger-KatzMay 28, 2020
"In New York City, which has had the largest coronavirus outbreak in the United States, around 20 percent of the city’s residents have been infected by the virus as of early May" - using antibody testing
https://www.nytimes.com/interactive/2020/05/28/upshot/coronavirus-herd-immunity.html
“When will it be over?”: An introduction to viral reproduction numbers, R0 and Re
https://www.cebm.net/covid-19/when-will-it-be-over-an-introduction-to-viral-reproduction-numbers-r0-and-re/
R0, the Messy Metric That May Soon Shape Our Lives, Explained
‘R-naught’ represents the number of new infections estimated to stem from a single case. You may be hearing a lot about this.
https://www.nytimes.com/2020/04/23/world/europe/coronavirus-R0-explainer.html
The Novel Coronavirus, 2019-nCoV, is Highly Contagious and More Infectious Than Initially Estimated
https://www.medrxiv.org/content/10.1101/2020.02.07.20021154v1
COVID-19 R0: Magic number or conundrum?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7073717/
How Scientists Quantify the Intensity of an Outbreak Like COVID-19
An epidemiologist explains the term "R0" and how many people one person with the coronavirus can infect.
https://labblog.uofmhealth.org/rounds/how-scientists-quantify-intensity-of-an-outbreak-like-covid-19
Herd immunity to the coronavirus would require 50% of the US population to become immune — and we're 'a long way' from that, experts say
https://www.businessinsider.com/us-covid-19-herd-immunity-2020-4
Illustration of herd immunity below:
(from https://thecorrespondent.com/356/what-is-herd-immunity/47084934512-1a3805b9)
Graph (below)in article from Imperial College UK model approximately verifies, what data indicates at this point May 2020
https://www.nytimes.com/2020/03/16/us/coronavirus-fatality-rate-white-house.html
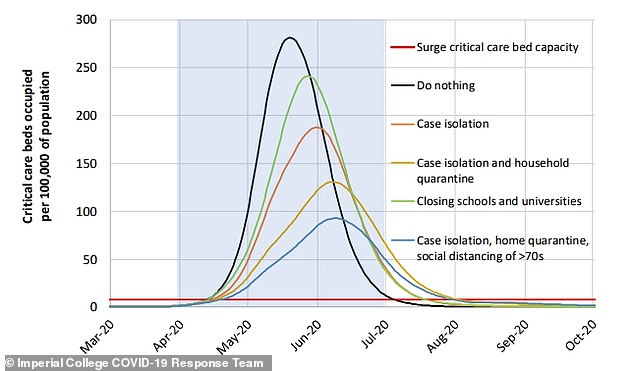
Below are the R(0) range of values for different viruses, and how transmitted, plus I calculated for 4 viruses the herd immunity range based on the R(0) values.
https://www.researchgate.net/figure/Values-of-R0-of-well-known-infectious-diseases_tbl2_340317966
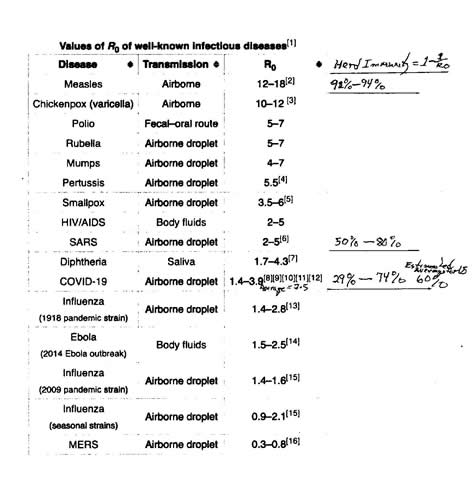
Possible model senario: graph showing bounces due to periodic control measures being relaxed. until September 2021,
https://science.sciencemag.org/content/367/6485/1414.2
From pandemic to endemic: this is how we might get back to normal
Covid-19 is unlikely to be eradicated, experts say, but societies in the past have learned to live with diseases
https://www.theguardian.com/us-news/2021/dec/05/covid-19-from-pandemic-to-endemic-this-is-how-we-might-get-back-to-normal
16 February 2021
The coronavirus is here to stay — here’s what that means
A Nature survey shows many scientists expect the virus that causes COVID-19 to become endemic, but it could pose less danger over time.
https://www.nature.com/articles/d41586-021-00396-2
The Risks - Know Them - Avoid Them
https://youtu.be/bB2kLZhqf5I covid-19 riskier and safer places - short video with some of the below information
Subsections of article
Where are people getting sick?
How much Virus is released into the environment?
Remember the formula: Successful Infection = Exposure to Virus x Time
What is the role of asymptomatic people in spreading the virus?
So now let’s get to the crux of it. Where are the personal dangers from reopening?
Commonality of outbreaks
Very Brief summary of article (read full article, at the link below, it tells so much more important information)
The main sources for infection are home, workplace, public transport, social gatherings, and restaurants. This accounts for 90% of all transmission events. In contrast, outbreaks spread from shopping appear to be responsible for a small percentage of traced infections. (Ref)
Importantly, of the countries performing contact tracing properly, only a single outbreak has been reported from an outdoor environment (less than 0.3% of traced infections). From a study of more than 7,300 cases in China.
Other interesting data from the reports below:
1 minute of loud speaking could create at least 1,000 respiratory droplets that remain suspended in the air for up to 8 minutes.
A study in March in The New England Journal of Medicine found that under laboratory conditions, the virus can survive for up to three days on some surfaces, such as plastic and steel, and on cardboard for up to 24 hours.
Other studies reported finding the virus on air vents in hospital rooms and on computer mice, sickbed handrails and doorknobs.
Many people grew worried that by touching a surface that had been covered in droplets by an infected person, and then touching their own mouth, nose or eyes, they then would contract the virus.
Other scientists commenting on these studies said virus on these surfaces might degrade more quickly. The Centers for Disease Control and Prevention has said since March that contaminated surfaces are “not thought to be the main way” the virus spreads. The main driver of infection is thought to be directly inhaling droplets released when an infected person sneezes, coughs, sings or talks. The C.D.C. recently made changes to its website to make this message even more explicit.
A few things are known about conditions that do or do not favor the virus. The ultraviolet rays in sunlight help destroy the virus on surfaces and some studies have shown a small effect from humidity. It seems to last longest on hard surfaces like plastic and metal. It won’t survive in pool or lake or seawater. Wind disperses it. Risk of transmission is lower outdoors than indoors.
“I think outdoors is so much better than indoors in almost all cases,” said Linsey Marr, an engineering professor and aerosol scientist at Virginia Tech. “There’s so much dilution that happens outdoors. As long as you’re staying at least six feet apart, I think the risk is very low.”
Pandemic life is safer outdoors, in part, because even a light wind will quickly dilute the virus. If a person nearby is sick, the wind will scatter the virus, potentially exposing nearby people but in far smaller quantities, which are less likely to be harmful.
“The virus load is important,” said Eugene Chudnovsky, a physicist at Lehman College and the City University of New York’s Graduate Center. “A single virus will not make anyone sick; it will be immediately destroyed by the immune system. The belief is that one needs a few hundred to a few thousand of SARS-CoV-2 viruses to overwhelm the immune response.”
https://www.erinbromage.com/post/the-risks-know-them-avoid-them
https://www.nytimes.com/article/coronavirus-facts-history.html (June 2 2020)
https://www.erinbromage.com/post/flying-in-the-age-of-covid-19
Air pollution and Covid-19 health risk.
Air pollution includes not only industrial, agricultural, car and truck driving pollution, also included is fireplace and other wood and coal and charcol burning.
One recent study found that even small increases in fine particulate matter, known as PM2.5, have had an outsized effect in the US. An increase of just 1 microgram per cubic metre corresponded to a 15% increase in Covid-19 deaths, according to the researchers, led by Xiao Wu and Rachel Nethery at the at the Harvard University T.H. Chan School of Public Health. ...
https://www.bbc.com/future/article/20200427-how-air-pollution-exacerbates-covid-19
It is good to keep in mind that many biological processes operate on a probability curve, binary answers (yes or no or positive/negative) tend to be over-simplifications that the public wants. Among other things, this aspect of biology shows up in tests for infection diseases like covid-19, for both the antibodies tests and the PCR tests for the virus itself.
For example: a probability curve shows up in the PCR test for the presence of covid-19 viral RNA, but must be reduced to a negative or positive result. To a degree, one consequence is the Chinese version of the RT-PCR test had a conspicuous rate of false negative results, likely missing between 15% and 29% of patients with COVID-19, according to a paper by University of Texas Health Science Center.
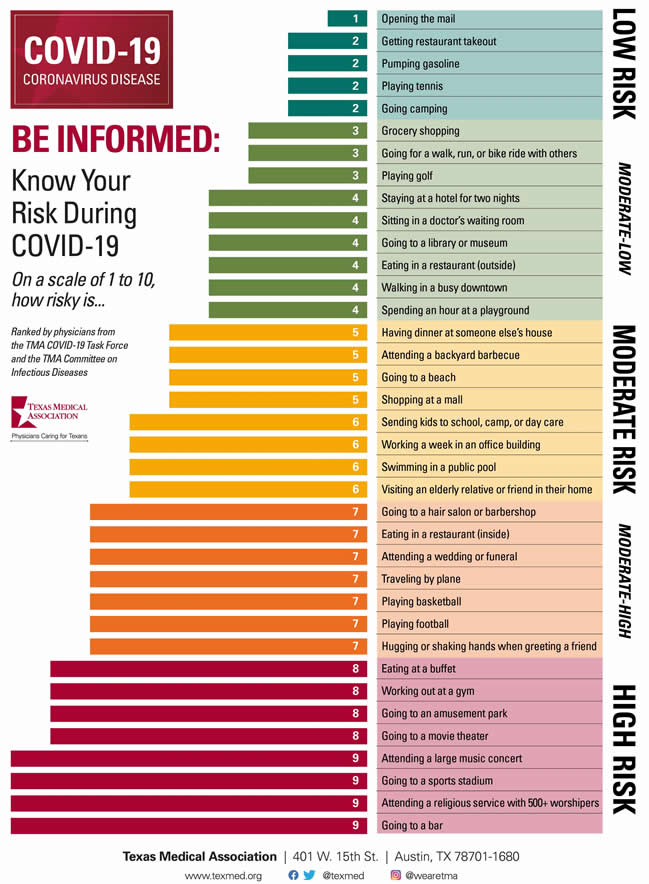
Below Parody but partially true risk chart from:
https://twitter.com/xkcdcomic/status/1283437923421937666
https://imgs.xkcd.com/comics/covid_risk_chart_2x.png
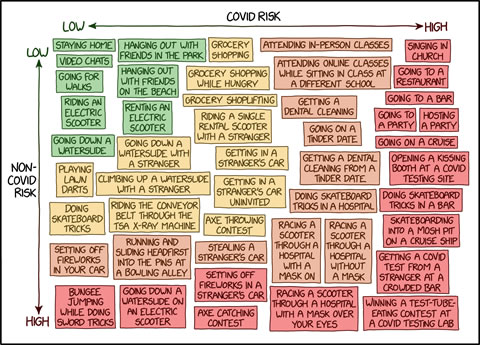
The science of airborne spread of covid
Transmission of Viruses in Droplets and Aerosols (part 1)
good illustrations in this lecture
Part 1 covers virus size and the size distributions of respiratory droplets and aerosols that carry viruses. Since making this video, I added the following text to the slide on transmission modes, addressing the definition of droplet (larger than 5 microns) vs. aerosol (smaller than 5 microns)
Prof. Linsey Marr 17 minutes
https://www.youtube.com/watch?v=dD1gKaaQg6k
Transmission of Viruses in Droplets and Aerosols (part 2)
Prof. Linsey Marr 12 minutes
Aerosol dynamics: transport, transformation, and removal by gravitational settling, ventilation, and inactivation of viruses
https://www.youtube.com/watch?v=JaN2PMgBQfI
Transmission of Viruses in Droplets and Aerosols (part 3)
Prof. Linsey Marr 11 minutes
https://www.youtube.com/watch?v=9FqnnTKSAzU
Transmission of Viruses in Droplets and Aerosols (part 4)
Prof. Linsey Marr 14 minutes
How masks work and latest info (as of 26 March 2020) about SARS-CoV-2. I should point out that the final slide on masks shows results from a laboratory study with masks on a manikin. In the real-world, the reduction could be lower.
https://www.youtube.com/watch?v=rCRdtTMHNXE
COVID 10: Is COVID-19 an airborne disease? Will we all need to wear face-masks against SARS-CoV-2?
There seems to be a lot of confusion in the droplet versus aerosol discussion and how these relate to the spread of COVID-19. Is it airborne and inhaled or droplet based via fomites and hands? The uncomfortable truth is that we have evidence for both modes.
https://www.youtube.com/watch?v=JJpt6Bse0j8
Part 3:
As of March 2020, below is detailed look at current Emergency Room and ICU standard treatment of Covid-19
Rejoice, medical peeps. This is all you need to know to date. (using somewhat standard practice ICU approach) (Borrowed from Mary Alice ... who borrowed it from another place )
"I am an ER MD in New Orleans. Class of 98. Every one of my colleagues have now seen several hundred Covid 19 patients and this is what I think I know.
Clinical course is predictable.
2-11 days after exposure (day 5 on average) flu like symptoms start. Common are fever, headache, dry cough, myalgias(back pain), nausea without vomiting, abdominal discomfort with some diarrhea, loss of smell, anorexia, fatigue.
Day 5 of symptoms- increased SOB, and bilateral viral pneumonia from direct viral damage to lung parenchyma.
Day 10- Cytokine storm leading to acute ARDS and multiorgan failure. You can literally watch it happen in a matter of hours. 81% mild symptoms, 14% severe symptoms requiring hospitalization, 5% critical. Patient presentation is varied. Patients are coming in hypoxic (even 75%) without dyspnea.
I have seen Covid patients present with encephalopathy, renal failure from dehydration, DKA. I have seen the bilateral interstitial pneumonia on the xray of the asymptomatic shoulder dislocation or on the CT's of the (respiratory) asymptomatic polytrauma patient.
Essentially if they are in my ER, they have it. Seen three positive flu swabs in 2 weeks and all three had Covid 19 as well.
Somehow this ***** has told all other disease processes to get out of town. China reported 15% cardiac involvement. I have seen covid 19 patients present with myocarditis, pericarditis, new onset CHF and new onset atrial fibrillation. I still order a troponin, but no cardiologist will treat no matter what the number in a suspected Covid 19 patient.
Even our non covid 19 STEMIs at all of our facilities are getting TPA in the ED and rescue PCI at 60 minutes only if TPA fails. Diagnostic CXR- bilateral interstitial pneumonia (anecdotally starts most often in the RLL so bilateral on CXR is not required). The hypoxia does not correlate with the CXR findings. Their lungs do not sound bad.
Keep your stethoscope in your pocket and evaluate with your eyes and pulse ox. Labs- WBC low, Lymphocytes low, platelets lower then their normal, Procalcitonin normal in 95% CRP and Ferritin elevated most often. CPK, D-Dimer, LDH, Alk Phos/AST/ALT commonly elevated. Notice D-Dimer- I would be very careful about CT PE these patients for their hypoxia. The patients receiving IV contrast are going into renal failure and on the vent sooner.
Basically, if you have a bilateral pneumonia with normal to low WBC, lymphopenia, normal procalcitonin, elevated CRP and ferritin- you have covid-19 and do not need a nasal swab to tell you that. A ratio of absolute neutrophil count to absolute lymphocyte count greater than 3.5 may be the highest predictor of poor outcome. the UK is automatically intubating these patients for expected outcomes regardless of their clinical presentation. An elevated Interleukin-6 (IL6) is an indicator of their cytokine storm. If this is elevated watch these patients closely with both eyes.
Other factors that appear to be predictive of poor outcomes are thrombocytopenia and LFTs 5x upper limit of normal.
Disposition I had never discharged multifocal pneumonia before. Now I personally do it 12-15 times a shift. 2 weeks ago we were admitting anyone who needed supplemental oxygen. Now we are discharging with oxygen if the patient is comfortable and oxygenating above 92% on nasal cannula. We have contracted with a company that sends a paramedic to their home twice daily to check on them and record a pulse ox. We know many of these patients will bounce back but if it saves a bed for a day we have accomplished something.
Obviously we are fearful some won't make it back. We are a small community hospital. Our 22 bed ICU and now a 4 bed Endoscopy suite are all Covid 19. All of these patients are intubated except one. 75% of our floor beds have been cohorted into covid 19 wards and are full. We are averaging 4 rescue intubations a day on the floor.
We now have 9 vented patients in our ER transferred down from the floor after intubation. Luckily we are part of a larger hospital group. Our main teaching hospital repurposed space to open 50 new Covid 19 ICU beds this past Sunday so these numbers are with significant decompression.
Today those 50 beds are full. They are opening 30 more by Friday. But even with the "lockdown", our AI models are expecting a 200-400% increase in covid 19 patients by 4/4/2020. Treatment Supportive worldwide 86% of covid 19 patients that go on a vent die. Seattle reporting 70%. Our hospital has had 5 deaths and one patient who was extubated. Extubation happens on day 10 per the Chinese and day 11 per Seattle. Plaquenil which has weak ACE2 blockade doesn't appear to be a savior of any kind in our patient population.
Theoretically, it may have some prophylactic properties but so far it is difficult to see the benefit to our hospitalized patients, but we are using it and the studies will tell.
With Plaquenil's potential QT prolongation and liver toxic effects (both particularly problematic in covid 19 patients), I am not longer selectively prescribing this medication as I stated on a previous post. We are also using Azithromycin, but are intermittently running out of IV. Do not give these patient's standard sepsis fluid resuscitation. Be very judicious with the fluids as it hastens their respiratory decompensation. Outside the DKA and renal failure dehydration, leave them dry. Proning vented patients significantly helps oxygenation. Even self proning the ones on nasal cannula helps. Vent settings- Usual ARDS stuff, low volume, permissive hypercapnia, etc. Except for Peep of 5 will not do. Start at 14 and you may go up to 25 if needed. Do not use Bipap- it does not work well and is a significant exposure risk with high levels of aerosolized virus to you and your staff. Even after a cough or sneeze this virus can aerosolize up to 3 hours.
The same goes for nebulizer treatments. Use MDI. you can give 8-10 puffs at one time of an albuterol MDI. Use only if wheezing which isn't often with covid 19. If you have to give a nebulizer must be in a negative pressure room; and if you can, instruct the patient on how to start it after you leave the room.
Do not use steroids, it makes this worse. Push out to your urgent cares to stop their usual practice of steroid shots for their URI/bronchitis.
We are currently out of Versed, Fentanyl, and intermittently Propofol. Get the dosing of Precedex and Nimbex back in your heads.
One of my colleagues who is a 31 yo old female who graduated residency last may with no health problems and normal BMI is out with the symptoms and an SaO2 of 92%. She will be the first of many.
I PPE best I have. I do wear a MaxAir PAPR the entire shift. I do not take it off to eat or drink during the shift. I undress in the garage and go straight to the shower. My wife and kids fled to her parents outside Hattiesburg. The stress and exposure at work coupled with the isolation at home is trying. But everyone is going through something right now. Everyone is scared; patients and employees. But we are the leaders of that emergency room. Be nice to your nurses and staff. Show by example how to tackle this crisis head on. Good luck to us all."
Part 4:
A somewhat detailed look at how the virus might be causing extreme hypoxia (lack of oxygen) and death, if viral proteins are interfering with hemoglobin's role in oxygen transport, and if this occurs before the cytokine storm and the destruction of the lungs and other organs.
B) An altered less invasive ICU protocol, from standard ICU treatment, if this is the case.
C)Following the details of the above theory is an newly emerging theory related to covid-19 role in causing strokes by invading endothelial cells.
Mounting evidence for different Covid-19 treatments - see 6 min video from ER doctor at below link, who points out the problems with the current ICU approach.
https://medium.com/@andrewt3000/covid-19-and-hypoxemia-697bc8a19bae
Below are science articles with information on possibly how the virus is causing hypoxia and altering treatment. The article below all the links is written (somewhat) in layperson's terms:
https://chemrxiv.org/articles/COVID19_Disease_ORF8_and_Surface_Glycoprotein_Inhibit_Heme_Metabolism_by_Binding_to_Porphyrin/11938173
The below theory related to Hemoglobin, seem to gradually be losing favor to the 3rd theory, involving endothelial cells, presented after the heme theory.
Covid-19 Biological Perspective -Part 2
https://medium.com/@jain.sm/covid-19-biological-perspective-part-2-d9d274654fe8
COVID-19: Attacks the 1-Beta Chain of Hemoglobin and Captures the Porphyrin to Inhibit Human Heme Metabolism
https://www.reddit.com/r/COVID19/comments/fs58u7/covid19_attacks_the_1beta_chain_of_hemoglobin_and/
The original article supporting the Heme theory
http://bigagbigchem.org/babc/covid19chinaHemeorginalpaper.pdf
Summary of original paper
https://chemrxiv.org/articles/COVID-19_Disease_ORF8_and_Surface_Glycoprotein_Inhibit_Heme_Metabolism_by_Binding_to_Porphyrin/11938173
Critique of above paper
https://healthfeedback.org/claimreview/claim-that-sars-cov-2-binds-to-hemoglobin-in-red-blood-cells-unsupported-and-implausible-andrew-gaiziunas/
Brief summary of the above heme theory:
It appears the convid-19 virus is hijacking components of Hemoglobin around day 8 or greater in the disease course and preventing oxygenation, which causes all the destructive effects of hypoxia to body organs, which in later stages may cause a cytokine storm, which sets up the destructive hyper inflammatory immune system reaction.
In the part of the population, which has a very robust immune system (mainly younger part of the population) the antibody response seems to limit the proliferation of the virus before major hypoxia damage can occur.
In weaker immune systems:
Until a safe antiviral drug for covid-19 is developed: 1) then limiting the virus proliferation with what is safely available in the early stages 2) treating the hypoxia as soon as possible with oxygenation so the immune system response has time to take hold before major organ destruction happens.
Apr 7 More detailed summary of the main points of the heme theory of covid-19 causing hypoxia.
COVID-19 glycoproteins bond to the heme groups, and in doing so the oxidative iron ion is “disassociated” (released) from red blood cells.
Without the iron ion, hemoglobin can no longer bind to oxygen, rendering the red blood cells useless.
It is very likely that this is more the case, rather than developing a form of ARDS or pneumonia.
Many doctors are starting to believe that they are operating under a false notion of pneumonia, & possibly treating the wrong symptoms on a systematic basis throughout the country.
Ventilators may not be treating the root cause, as many of the patient’s lungs aren’t ‘tiring out’, they’re pumping just fine.
It is instead that the affected hemoglobin have been stripped of their ability to carry oxygen, resulting in hypoxia.
The body compensates for this lack of O2 carrying capacity by having your kidneys release hormones like erythropoietin, which tell your bone marrow factories to ramp up production on new red blood cells with freshly made and fully functioning hemoglobin.
This is the reason you find elevated hemoglobin and decreased blood oxygen saturation as one of the 3 primary indicators of poor prognosis for a particular patient.
Reactive oxygen species in erythrocytes are generated through heme degradation.
Displaced Fe, released after viral attack on hemoglobin, is thought to be responsible for extensive free radical damage to the lungs.
If the patient’s immune system doesn’t fight off the virus in time before their blood oxygen saturation drops too low, ventilator or no ventilator, organs start shutting down.
The only way to try to keep them going is by delivering oxygen or a transfusion of red blood cells.
In conclusion, Physicians may need to re-evaluate treatment options and their basis-of-understanding for COVID-19, in light of its newly realized ability to induce hypoxemia in the patient.
This theory advocates:
1) Lower the covid-19 viral load with antivirals that work (currently easier said than done)
2) Treating the hypoxia more aggressively and sooner, but in a less harmful way than current intubation plus ventilator use.
A more detailed article presented in layperson terms of the heme theory of covid-19 causing hypoxia is at the below link
http://bigagbigchem.org/babc/Hemetheoryarticle.html
The 3rd theory is that the new coronavirus invading endothelial cells and causing numerous blood clots.
Below are quotes from recent publications and links to the articles.
"The virus seems to be causing increased clotting in the large arteries, leading to severe stroke,"
Our report shows a seven-fold increase in incidence of sudden stroke in young patients during the past two weeks. Most of these patients have no past medical history and were at home with either mild symptoms (or in two cases, no symptoms) of COVID," he added.
...
Sharon Fox, MD, PhD, agrees with him. She’s a pathologist at Louisiana State University Health in New Orleans and has been doing autopsies on patients who have died with COVID-19. She’s finished 20 cases so far, and they share something in common: They are riddled with blood clots in the smallest vessels of the body. Lungs seem to be especially hard-hit. There, clots appear to have cut off blood flow to the small air sacs where blood cells would be exchanging oxygen and carbon dioxide.
“There’s no ability for the blood to flow through and exchange oxygen like it should,” she says.
...
A research letter published this week in The Lancet reported evidence of viral bodies of the new coronavirus invading endothelial cells. The endothelium is the lining of our blood vessels. It directs important functions of the vascular system like clotting and swelling.
...
Images captured with an electron microscope found traces of the coronavirus in endothelial cells in the heart, kidney, small bowel, and lung -- pretty much all over the body. Researchers collected the tissues during autopsies of three patients who died of COVID-19.
Blood Clots Are Another Dangerous COVID-19 Mystery
https://www.webmd.com/lung/news/20200424/blood-clots-are-another-dangerous-covid-19-mystery
Young and middle-aged people, barely sick with covid-19, are dying from strokes
Doctors sound alarm about patients in their 30s and 40s left debilitated or dead. Some didn’t even know they were infected.
https://www.washingtonpost.com/health/2020/04/24/strokes-coronavirus-young-patients/
COVID-19 causing blood clots, sudden strokes in young adults, doctors say
https://www.ctvnews.ca/health/coronavirus/covid-19-causing-blood-clots-sudden-strokes-in-young-adults-doctors-say-1.4910674
Coronavirus Pandemic Update 63: Is COVID-19 a Disease of the Endothelium (Blood Vessels and Clots)?
critical care specialist Roger Seheult, MD explains the underlying biochemistry that points to the mechanism of how Covid-19 seems to be effecting the endothelium via oxidative stress
also, The Role of Zinc, Copper, Manganese and Iron in this biochemistry
https://www.youtube.com/watch?v=Aj2vB_VITXQ
COVID-19 Can Attack the Heart in Addition to the Lungs
5-20-20
https://www.healthline.com/health-news/how-covid-19-triggers-heart-conditions
Part 5)
Below is a day by day narration of symptoms of a person's bout with covid-19.
The below person is a
healthy 40 year old with no prior health problems. (shown as a photo for her phone text narration)
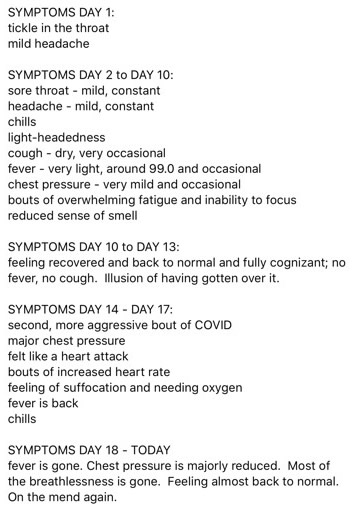
6)
If you have survived being infected by covid-19, are you now immune to being reinfected? Not necessarily.
Below are 2 good articles with some details about covid-19 immunity and testing for immunity.
What Covid-19 antibody tests say — and don’t say — about immunity
A positive antibody test doesn’t yet mean you’re immune to Covid-19.
https://www.vox.com/science-and-health/2020/4/28/21237922/antibody-test-covid-19-immunity
The below article in the medical journal Lancet, covers immunity and a number of other important aspects of covid-19.
What policy makers need to know about COVID-19 protective immunity
Published:April 27, 2020
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30985-5/fulltext
A new stain for covid-19 confounds the immunity issue.
Scientists Say a Now-Dominant Strain of the Coronavirus Appears to Be More Contagious Than Original
May 5, 2020
The mutation identified in the new report affects the now infamous spikes on the exterior of the coronavirus, which allow it to enter human respiratory cells. The report’s authors said they felt an “urgent need for an early warning” so that vaccines and drugs under development around the world will be effective against the mutated strain.
...
If the pandemic fails to wane seasonally as the weather warms, the study warns, the virus could undergo further mutations even as research organizations prepare the first medical treatments and vaccines. Without getting on top of the risk now, the effectiveness of vaccines could be limited. Some of the compounds in development are supposed to latch onto the spike or interrupt its action. If they were designed based on the original version of the spike, they might not be effective against the new coronavirus strain, the study’s authors warned.
...
Scientists at major organizations working on a vaccine or drugs have told The Times that they are pinning their hopes on initial evidence that the virus is stable and not likely to mutate the way influenza virus does, requiring a new vaccine every year. The Los Alamos report could upend that assumption.
...
https://readersupportednews.org/news-section2/318-66/62768-focus-scientists-say-a-now-dominant-strain-of-the-coronavirus-appears-to-be-more-contagious-than-original
Do Your Genes Predispose You to COVID-19?
Individual differences in genetic makeup may explain our susceptibility to the new coronavirus and the severity of the disease it causes
By Loïc Mangin on April 30, 2020
Brief summary of article below:
Men made up 73 percent of severe cases of COVID-19 in intensive care in France, according to a national survey published April 23. Behavioral and hormonal differences may be partially responsible. But genes may also factor into the mix. Unlike men, women have two X chromosomes and so carry double the copies of the gene TLR7, a key detector of viral activity that helps boost immunity.
...
The genetics of blood groups may offer some insight into whether you are liable to be infected with the virus, in a severe way. In late March Peng George Wang of the Southern University of Science and Technology in China and his colleagues released the results of a preprint study—not yet peer-reviewed—that compared the distribution of blood types among 2,173 COVID-19 patients in three hospitals in the Chinese cities of Wuhan and Shenzhen with that of uninfected people in the same areas. Blood type A appears to be associated with a higher risk of contracting the virus, whereas type O offers the most protection for reasons that have yet to be determined.
...
read article below for additional genetic markers and explainations.
https://www.scientificamerican.com/article/do-your-genes-predispose-you-to-covid-19/
This video explains blood types and then presents the findings of the Chinese study. Where A type has proportionally more deaths, than O type, even when you control for the different proportions of types in the population and age and gender.
https://www.youtube.com/watch?v=JICtQjrn9fE
This paper shows the actual percentages and sample size. Of those who died 41% had type A and 25% had type O.
https://www.coronavirustoday.com/blood-type-people-might-need-strengthen-personal-protections-sars-cov-2
Why COVID-19 kills some people and spares others. Here's what scientists are finding.
https://www.livescience.com/why-covid-19-coronavirus-deadly-for-some-people.html
Why Does the Coronavirus Hit Men Harder? A New Clue
Women produce a more powerful immune response than do men, a new study finds.
By Apoorva Mandavilli
Published Aug. 26, 2020 Updated Aug. 27, 2020, 9:33 a.m. ET
The coronavirus may infect anyone, young or old, but older men are up to twice as likely to become severely sick and to die as women of the same age.
Why? The first study to look at immune response to the coronavirus by sex has turned up a clue: Men produce a weaker immune response to the virus than do women, the researchers concluded.
The findings, published on Wednesday in Nature, suggest that men, particularly those over age 60, may need to depend more on vaccines to protect against the infection.
...
https://www.nytimes.com/2020/08/26/health/coronavirus-men-immune.html
Part 7:
NEWS FEATURE 15 May 2020
15 drugs being tested to treat COVID-19 and how they would work
Scientists have been investigating a plethora of drugs that may be repurposed to fight COVID-19. The hope is that of the 15 drugs listed here, some could be discovered as a treatment for this disease.
One of Note is Famotidine
"The over-the-counter H2 receptor antagonist heartburn medication famotidine is also been investigated as a possible treatment, after Michael Callahan and colleagues in China reported that patients in Wuhan who happened to be taking heartburn medication seemed less likely to die from or to be intubated during severe COVID-19. These observations have been published as a preprint, but have yet to be peer-reviewed.
...Malone says his team is enthusiastic about the drug because of its low cost, low toxicity and bioavailability."
https://www.nature.com/articles/d41591-020-00019-9
Heartburn Drug Decreased COVID-19 Disease Fatalities
Famotidine is a Pepcid ingredient which treats heartburn and gastric acid
https://www.precisionvaccinations.com/famotidine-pepcid-ingredient-which-treats-heartburn-and-gastric-acid
"The idea came from something Michael Callahan, an infectious disease doctor at Massachusetts General Hospital, saw when he was working in the Chinese city of Wuhan just as the coronavirus epidemic began to take off there.
Doctors noticed many of the people surviving COVID-19 tended to be poorer, he told a reporter with the journal Science in an article published in its news section Sunday. They noticed that many of the survivors had chronic heartburn and took famotidine rather than omeprazole, sold in the United States as Prilosec, which is much more expensive."
https://www.usatoday.com/story/news/health/2020/04/28/pepcid-treat-covid-19-theory-trending-online-coronavirus/3043325001/
Can Pepcid treat COVID-19?
With clinical trials ongoing, doctors try to unravel how famotidine could be working to fight the disease caused by SARS-CoV-2
by Bethany Halford
June 15, 2020 | APPEARED IN VOLUME 98, ISSUE 25
https://cen.acs.org/pharmaceuticals/Pepcid-treat-COVID-19/98/i25
Two drugs currently undergoing clinical trials for treating covid-19
Remdesivir and Hydroxychloroquine
A closer look at two drugs currently undergoing clinical trials for treatment of Covid-19.
In very brief summary, both drugs show some promise in small scale trials, so far only one using, Hydroxychloroquine, has any controls (placebo included testing). Done in China, not peer reviewed yet.
Larger studies for both drugs, with controls, are in process as of 4-12-2020, but not completed and peer reviewed.
The links included below, except for one, were picked because they included the drugs mechanism, and in all cases, except one, came from science based publications, written with layperson language in mind.
Remdesivir
What can initial remdesivir data tell us about tackling COVID-19?
Critical study of Gilead’s Covid-19 drug shows patients are responding to treatment, NIH says
By Matthew Herper @matthewherper and Adam Feuerstein @adamfeuerstein
April 29, 2020
https://www.statnews.com/2020/04/29/gilead-says-critical-study-of-covid-19-drug-shows-patients-are-responding-to-treatment/
Gilead Sciences’ antiviral is in multiple late-stage trials to treat coronavirus infections. Don’t expect a home run, say infectious disease experts
https://cen.acs.org/biological-chemistry/infectious-disease/initial-remdesivir-data-tell-us/98/i13
Virus Outbreak: First results for Gilead’s remdesivir show promise
https://www.taipeitimes.com/News/front/archives/2020/04/12/2003734454
A Paper Raises Some Safety Concerns for Gilead’s COVID-19 Treatment
https://www.biospace.com/article/a-paper-raises-some-safety-concerns-for-gilead-s-covid-19-treatment/
Hydroxychloroquine
Can Hydroxychloroquine and Chloroquine Be Used to Treat Coronavirus (COVID-19)?
https://www.goodrx.com/blog/coronavirus-medicine-chloroquine-hydroxychloroquine-as-covid19-treatment/
Study finds no hydroxychloroquine effect on death, severe COVID-19
also shown to increase cardiac adverse events
https://www.cidrap.umn.edu/news-perspective/2020/05/study-finds-no-hydroxychloroquine-effect-death-severe-covid-19
Why scientists are studying if chloroquine could treat coronavirus (one can see why this drug may help if the emerging theory related to covid-19 interfering with Hemoglobin’s oxygen transport role, proves to be correct)
A close look at why this old malaria drug could be promising for COVID-19
https://www.asbmb.org/asbmb-today/science/032820/why-scientists-are-studying-if-chloroquine-could-t
Results from a Controlled Trial of Hydroxychloroquine for COVID-19
https://www.contagionlive.com/news/results-from-a-controlled-trial-of-hydroxychloroquine-for-covid19
How Does Hydroxychloroquine and Azithromycin Combination Therapy Measure Up For COVID-19 Treatment?
https://www.contagionlive.com/news/how-does-hydroxychloroquine-and-azithromycin-combination-therapy-measure-up-for-covid19-treatment
Heartburn Drug (famotidine) May Have Potential Against COVID-19
June 10, 2020
https://www.cuimc.columbia.edu/news/heartburn-drug-may-have-potential-against-covid-19
IDSA Updates COVID-19 Treatment Guidelines (drugs)
JUNE 26, 2020
https://www.idse.net/Covid-19/Article/06-20/IDSA-Updates-COVID-19-Treatment-Guidelines/58829
Related to Covid-19 Vaccine Development
Why we might not get a coronavirus vaccine
Politicians have become more cautious about immunisation prospects. They are right to be
...Vaccines are simple in principle but complex in practice. The ideal vaccine protects against infection, prevents its spread, and does so safely. But none of this is easily achieved, as vaccine timelines show....
https://www.theguardian.com/world/2020/may/22/why-we-might-not-get-a-coronavirus-vaccine
The Risks of Rushing a COVID-19 Vaccine
Telescoping testing time lines and approvals may expose all of us to unnecessary dangers
By William A. Haseltine on June 22, 2020
https://www.scientificamerican.com/article/the-risks-of-rushing-a-covid-19-vaccine/
Moderna's vaccine genetic alterations passed down to future generations?
Almost no one understands what’s at stake: Pharma has 80 COVID vaccines in development, but Gates & Fauci pushed Moderna’s “Frankenstein jab” to the front of the line.
Scientists & ethicists are sounding alarms. The vaccine uses a new, untested, and very controversial experimental RNA technology that Gates has backed for over a decade. Instead of injecting an antigen & adjuvant as with traditional vaccines, Moderna plugs a small piece of coronavirus genetic code into human cells, altering DNA throughout the human body and reprogramming our cells to produce antibodies to fight the virus. MRNA vaccines are a form of genetic engineering called “germ line gene editing”. Moderna’s genetic alterations are passed down to future generations.
In January in The Geneva Statement the world’s leading ethicists and scientists called for an end to this kind of experimentation.
Moderna has never brought a product to market, proceeded through clinical trials, or had a vaccine approved by FDA. Despite Gates’ investments, the company was teetering on bankruptcy with $1.5 billion debt before COVID. Fauci’s support won the company an astonishing $483 million in federal funds to accelerate development. Dr. Joseph Bolen, Moderna’s former R&D Chief, expressed shock at Fauci’s bet. ”I don’t know what their thinking was”, he told CNN, “When I read that, I was pretty amazed”. Moderna and Fauci launched federally-funded human trials on March 3rd in Seattle. Dr Peter Hotez warns of potentially fatal consequences from skipping animal studies.
“If there is immune enhancement in animals, that’s a show-stopper”. Dr Suhab Siddiqi, Moderna’s Ex-Director of Chemistry, told CNN, “I would not let the [vaccine] be injected in my body. I would demand: Where is the toxicity data?”
Former NIH Scientist Dr. Judy Mikovits says it's criminal to test MRNA vaccines on humans. “MRNA can cause cancers and other dire harms that don’t surface for years.”
As precautions, Moderna ordered trial participants to avoid unprotected sex or sperm donations & Fauci directed that all COVID vaccines to be protected by blanket immunity.
Gates hopes to sell his experimental gene-altering technology to all 7 billion humans & transform our species into GMOs.”#transhumanism Are you ready for this?
He experienced a severe reaction to Moderna’s Covid-19 vaccine candidate. He’s still a believer
May 26, 2020
https://www.statnews.com/2020/05/26/moderna-vaccine-candidate-trial-participant-severe-reaction/
Moderna Vaccine Human 2.0 - Dr. Carrie Madej
https://www.youtube.com/watch?v=ti3x7DBIkrI
Here’s why we can’t rush a COVID-19 vaccine
Patrick Boyle , Staff Writer
March 31, 2020
https://www.aamc.org/news-insights/here-s-why-we-can-t-rush-covid-19-vaccine
The challenges of developing a safe and effective COVID-19 vaccine
May 12, 2020
Baylor College of Medicine
https://www.sciencedaily.com/releases/2020/05/200512151956.htm
Part 8)
5 ways coronavirus could help humanity survive the ecological crisis (short article)
https://ecohustler.com/nature/5-ways-coronavirus-could-help-humanity-survive-the-ecological-crisis/
b)
The covid-19 virus is attempting to teach us a lesson, about how we live. Unfortunately, the major media is not listening.
This link is to a less then 5 minute video with much of the same information as below, but includes additional images
https://youtu.be/8I3c8gJNMXI
As author Arundhati Roy says “The Pandemic Is a Portal” …”it offers us a chance to rethink the doomsday machine we have built for ourselves. Nothing could be worse than a return to normality.” …”we can walk through lightly, with little luggage, ready to imagine another world. And ready to fight for it.”
excerpts from: https://www.yesmagazine.org/video/coronavirus-pandemic-arundhati-roy/
The below articles show how the two great threats to humans are directly linked to how we treat wild and domestic animals.
The below articles go through the specifics of how and what we need to change.
How humans created a pandemic ‘highway’
The coronavirus shows that what we’re doing to animals is killing us, too.
By Viveca Morris
Associate Research Scholar in Law and Executive Director, Law, Ethics & Animals Program at Yale Law School
https://enewspaper.latimes.com/infinity/article_share.aspx?guid=29e450b5-3b8e-42ae-9c39-0e0ebcc69cd5
Neuroepidemiology
Factory Farms Should Be 'Discontinued' To Protect Humans, Says Scientists In New Paper
'We should rapidly evolve to eating other forms of protein that are safer for humans'
...
From a neuropsychiatric perspective, there are obvious signs of global psychological distress related to social isolation and fears of illness, death, and countless uncertainties about the future [3]. Less attention has been given to neurological manifestations including headache, anosmia, ageusia, ataxia, paresthesia, ischemic stroke, seizures, and various encephalopathies, collectively occurring in up to nearly 40% of hospitalized COVID-19 patients in early series. Encephalopathies have been more likely to occur in severely ill patients and have included at least one case of documented viral encephalitis with SARS-CoV-2 in the cerebrospinal fluid [4].
...
full article at:
https://www.karger.com/Article/FullText/508654
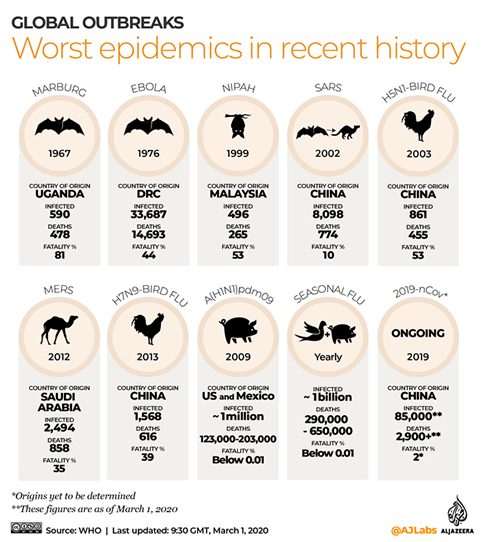
"A widely cited 2006 report by the United Nations Food and Agriculture Organization, Livestock’s Long Shadow, estimates that 18 percent of annual worldwide GHG emissions are attributable to cattle, buffalo, sheep, goats, camels, pigs, and poultry. But recent analysis by Goodland and Anhang finds that livestock and their byproducts actually account for at least 32.6 billion tons of carbon dioxide per year, or 51 percent of annual worldwide GHG emissions."
In other words 51% of the greatest threat to humans, man-made climate change is caused by animal agriculture.
https://awellfedworld.org/livestock-climate-advanced/
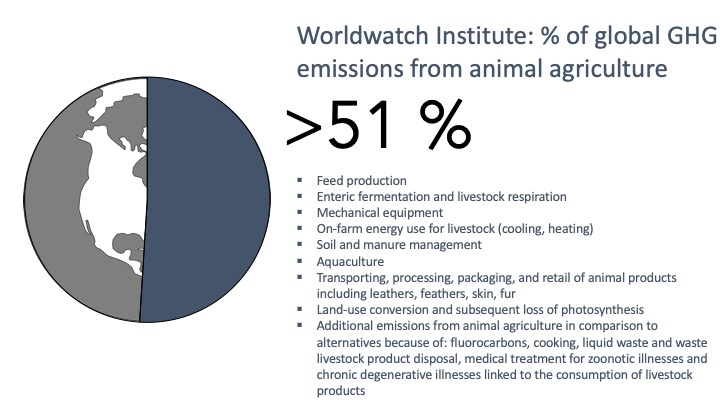
Meat And Agriculture Are Worse For The Climate Than Power Generation, Nobel Prize winning, Steven Chu Says:
https://www.forbes.com/sites/jeffmcmahon/2019/04/04/meat-and-agriculture-are-worse-for-the-climate-than-dirty-energy-steven-chu-says/#493e8bf811f9
Air pollution has dropped to unprecedented levels across the world as major cities and countries impose lockdown measures to curb the spread of the coronavirus.
As humans stay inside, the environment is temporarily changing: wild animals are roaming the streets and some typically smog-filled skies are clear.
Despite the rare glimpse of natural beauty like snow-crested mountains and clearer skylines, scientists warn against celebrating any short-term benefits from the air pollution drop as levels will rebound once global restrictions lift.
https://www.cnbc.com/2020/04/23/coronavirus-photos-show-effect-of-air-pollution-drops-from-global-lockdown.html
It's time to dismantle factory farms and get used to eating less meat
Gene Baur -- The Guardian
Slaughterhouses are a breeding ground for disease and hotspots for coronavirus, and dozens closed after thousands of workers became ill. President Trump ordered these operations open, and shielded them from legal liability for exposing disempowered workers to intolerable risks. At the same time, the government is spending $200m per month to support the meat and dairy industries, while agribusiness lobbies for more stimulus money to return to killing as normal. ...
https://www.theguardian.com/commentisfree/2020/may/19/its-time-to-get-used-to-eating-less-meat
c)
CORONAVIRUS - The Uncomfortable Truth -- 8 minute video
COVID-19 is not the first virus of its kind - nor is it likely to be the last. So why isn’t the media looking at the bigger - and more frightening - questions? Is there a much bigger global issue that the press is keeping silent about?
https://www.youtube.com/watch?v=vPdvq_6EphU
d) Doctor who predicted covid-19
Triple board-certified M.D., Dr. Zach Bush, joins Del in an evolutionary discussion on why Coronavirus is
https://www.youtube.com/watch?v=5RAtFBvKrVw
Zach Bush MD: Coronaviruses, Covid-19, Air & Soil & Pandemics Interview with Brian Rose (audio only) below link:
A lot of good information, that I believe is accurate. A couple of things where what Dr. Bush said, does not add up to solid facts on the RT-PCR test about false positives and negatives see this site section on testing, and the hypoxia that happens in severe forms of covid, is likely not similar to cyanide poisoning. One can see on this site about this in Part 1 of this site, success in UChicago avoidance of ventilators in severe covid by using high flow oxygen and proning contradicts the cyanide poisoning analogy.
https://www.youtube.com/watch?v=8G5kMhper2s
e)Biological weapons: gain of function (GOF) research with corona+ virus
Is the recent corona virus, COVID-19 a biological weapon?
Academic and Government laboratories worldwide are making already lethal viruses, including coronaviruses, more deadly in a process called gain of function (GOF).
https://www.uticaphoenix.net/2020/03/24/is-the-recent-corona-virus-covid-19-a-biological-weapon/
f) Profile of a killer: the complex biology powering the coronavirus pandemic
Scientists are piecing together how SARS-CoV-2 operates, where it came from and what it might do next — but pressing questions remain about the source of COVID-19
04 May 2020
https://www.nature.com/articles/d41586-020-01315-7
g) Chief Science Officer for Pfizer Says "Second Wave" Faked on False-Positive COVID Tests, "Pandemic is Over"
Updated on September 27, 2020
In a stunning development, a former Chief Science Officer for the pharmaceutical giant Pfizer says "there is no science to suggest a second wave should happen." The "Big Pharma" insider asserts that false positive results from inherently unreliable COVID tests are being used to manufacture a "second wave" based on "new cases."
Dr. Mike Yeadon, a former Vice President and Chief Science Officer for Pfizer for 16 years, says that half or even "almost all" of tests for COVID are false positives. Dr. Yeadon also argues that the threshold for herd immunity may be much lower than previously thought, and may have been reached in many countries already.
full story at:
https://hubpages.com/politics/Pfizer-Chief-Science-Officer-Second-Wave-Based-on-Fake-Data-of-False-Positives-for-New-Cases-Pandemic-is-Over
Part 9)
Some important lesser know details about Hand Washing and Mask wearing due to covid-19.
Hand washing: Why using so much soap given most urban and suburban water supplies are chlorinated, which kills many germs without soap?
The reason is: corona virus is a lipid (oil/fat based) with spikes, think of trying to wash off or dissolve coconut oil without using soap. It does not work very well. You need some medium that is a solvent to fat/oil like water plus soap or alcohol or the equivalents.
https://youtu.be/yoK2Ul00dAQ Short video with some of the below information, on Mask, Eye Glasses and Face Shields
The Mask (non medical workers masks) covering your mouth and nose when you might be within 6 feet of other people.
The 6 feet distance has some complexities shown in the below article related to wind speed.
https://aip.scitation.org/doi/pdf/10.1063/5.0011960
The mask is mainly to protect others from you in case you have covid-19 (with or without symptoms).
To facilitate protection for yourself, in addition to wearing a mask, some type of eye glasses (or eye shield) in addition to the mask is required. Your eyes are mucus membranes very vulnerable to expelled covid droplets. If your glasses fog up due to the mask, there are many methods shown on a web search to prevent fogging from happening.
If you know you can easily avoid, during your outing, being within 6 feet of other people, like a walk in an open space outdoors, then having the mask on all the time may have some health disadvantages (assuming it is not mitigating some spring allergies you may have.).
A few reasons not to have the mask on all the time, when you are sure you can social distance:
Having it on all the time tightly, will gradually cause pressure sores and/or skin irritations.
If you touch your cell phone to the mask it will be contaminated, a study shows that cell phones can be 10 times dirtier than a public toilet. If you are adjusting it, you are likely contaminating your face.
You are rebreathing some of your own respirated CO2. The problems discussed in medical literature are: with increased levels of CO2 because of rebreathing it, called hypercapnia, can lead to increased blood pressure, headaches, muscle twitches, rapid heart rate, chest pain, confusion, and fatigue.
http://thebetteroxygenmask.com/harmful-effects-of-rebreathing-carbon-dioxide-co2/
https://www.snopes.com/fact-check/masks-dangerous-health/
Do face masks really reduce coronavirus spread? Experts have mixed answers.
By Stephanie Pappas - Live Science Contributor April 12, 2020
https://www.livescience.com/are-face-masks-effective-reducing-coronavirus-spread.html
New Evidence Shows Wearing Face Mask Can Help Coronavirus Enter the Brain and Pose More Health Risk, Warn Expert
https://www.sciencetimes.com/articles/25713/20200518/wearing-face-masks-potentially-harmful-trap-exhaled-viruses-well-individuals.htm
Face masks pose serious risks to the healthy – Blaylock MD
https://accountingweekly.com/face-masks-pose-serious-risks-to-the-healthy-blaylock/
https://www.greenmedinfo.com/blog/dr-blaylock-face-masks-pose-serious-risks-healthy11
Preliminary report on surgical mask induced deoxygenation during major surgery
http://scielo.isciii.es/pdf/neuro/v19n2/3.pdf
I tested rebreathing my own CO2 by wearing my cotton mask, then using my Pulse Oximeter to measure by O2, it only lowered my O2 by 2% (from 98% to 96%) with 2 separate, 5 minute trials, it did raise my pulse rate by +5 and +8 in the 2 trials)
Be sure your mask is made with some breathable fabric like cotton, not nylon and polyester.
Wash it periodically with soap and water or it will end up with many germs and dirt.
Respiratory virus shedding in exhaled breath and efficacy of face masks
Published: 03 April 2020
https://www.nature.com/articles/s41591-020-0843-2
To complicate matters, below, is a South Korean study that indicates that masks have limited usefulness in preventing a covid-19 infection from spreading via cough.
Effectiveness of Surgical and Cotton Masks in Blocking SARS–CoV-2: A Controlled Comparison in 4 Patients
In Brief:
During respiratory viral infection, face masks are thought to prevent transmission (1). Whether face masks worn by patients with coronavirus disease 2019 (COVID-19) prevent contamination of the environment is uncertain (2, 3). A previous study reported that surgical masks and N95 masks were equally effective in preventing the dissemination of influenza virus (4), so surgical masks might help prevent transmission of severe acute respiratory syndrome–coronavirus 2 (SARS–CoV-2).
Objective: To evaluate the effectiveness of surgical and cotton masks in filtering SARS–CoV-2.
In conclusion, both surgical and cotton masks seem to be ineffective in preventing the dissemination of SARS–CoV-2 from the coughs of patients with COVID-19 to the environment and external mask surface. 4-6-2020
https://www.acpjournals.org/doi/10.7326/M20-1342
There are many problems with the above South Korean study, some shown in the comments sections of the study. It does have value but with many caveats.
Besides a sample size of only 4 patients.
One of the ones, I observe, is to make in more relevant to a typical situation. A cough can travel as fast as 50 mph and expel almost 3,000 droplets, and study had the petri dish only 20 cm away, that is, less than 8 inches. It would have been important to include the more frequent transmission infection situation of talking, which is done typically at approximately 61 cm (24 inches).
In the comments on the peer reviewed sections, points out that the quanities of virus measured in the petri dish likely are below the level of conveying infection.
Concerning the below video, in my opinion in this talk he does not make the case that Mask are not effective in limiting the spread of covid-19 (at least in the video).
He centers on the aersol vs droplet aspect, but does not support evidence of the ratio of droplets vs aerosolize particles, which is key to dismissing masks as limiting spread.
He does make an interesting presentation about seasonal death rate over many years, and raises and interesting point about why did California have the normal seasonal death rate, but other places have the covid-19 spike.
Former professor of physics at the University of Ottawa, Denis Rancourt, PhD, who just released a paper compiling seven studies on the science surrounding the effectiveness of masks.
https://www.youtube.com/watch?v=C1ODBTdNiG0&feature=share&fbclid=IwAR2aORByWZWcHidzrnM15sGNJMt_FXOFiVd9Oj2HIKOg8vQ6Lzl6xOH5_
https://www.rcreader.com/commentary/masks-dont-work-covid-a-review-of-science-relevant-to-covide-19-social-policy
July 9th 2020 Written By: Jim Meehan MD
During the COVID-19 pandemic, public health experts began telling us to follow a number of disease mitigation strategies that sounded reasonably scientific, but actually had little or no support in the scientific literature. Community wearing of masks was one of the more dangerous recommendations from our confused public health experts.
https://www.greenmedinfo.com/blog/healthy-people-should-not-wear-face-masks
Contradictory information on Mask materials in next to links
This says should be able to blow out a candle from 1 foot away with mask on. (I bet the medical writers creating the interview article reversed what was said)
http://med.stanford.edu/news/all-news/2020/06/stanford-scientists-contribute-to-who-mask-guidelines.html
These says to thin if can blow-out candle
https://globegazette.com/news/why-its-still-important-to-wear-a-face-mask/article_1d12d06c-81ce-51f3-b3ad-245a726c2a16.html
https://www.wbtv.com/2020/04/18/doctor-recommends-people-wear-masks-says-its-less-common-carolinas/
Flame test
https://www.afnor.org/en/faq-barrier-masks/
Also see,
That Office AC System Is Great — at Recirculating Viruses
https://nymag.com/intelligencer/2020/05/that-office-ac-system-is-great-at-recirculating-viruses.html
The CDC has some references shown on the bottom of the below article on their site, relevant to the issue.
https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover.html
Face Shields, plus and minus:
Are Face Shields The New Face Masks?
Elizabeth Gulino Last Updated May 26, 2020,
...
Last month, an opinion article published in JAMA argued that there could be many benefits to encouraging everyone to wear these face shields.
The three doctors who wrote the article made some pretty valid points: Face shields are easier to disinfect than cloth masks, they prevent the wearer from touching even more areas of their face than a cloth mask might, and they're easier to breathe in. People also tend to remove their cloth masks when they're talking to people. "The use of a face shield is also a reminder to maintain social distancing, but allows visibility of facial expressions and lip movements for speech perception," the researchers write.
They're also very effective at blocking exposure to the virus. In a simulation study, face shields were able to reduce immediate viral exposure by 96% when worn by a simulated health care worker within 18 inches of a cough.
https://www.refinery29.com/en-us/2020/05/9837787/face-shield-vs-mask-covid
Face Shields plus and minus chart

Covid-19: How the Virus Gets in and How to Block It: Aerosols, Droplets, Masks, Face Shields, & More
•Jul 16, 2020 UCSF Grand Rounds
UCSF School of Medicine
In this Covid-19 Medical Grand Rounds (July 16, 2020), three world experts discuss a variety of issues surrounding how the coronavirus moves from person to person, how best to block viral spread, and the potential that mask-wearing may not only prevent infection but also lead to a milder clinical course. The questions regarding aerosol vs. droplet transmission and the value of wearing masks and/or face shields are central to formulating public health strategies as well as to informing the personal decisions that each of us makes every day. The session is hosted by UCSF Department of Medicine chair Bob Wachter.
https://www.youtube.com/watch?v=Cio3rh6ta3w